Specialized medicine
Leaders in surgery and complex care.
Between St. Paul’s and Mount Saint Joseph Hospitals, our teams perform more than 10,000 surgical procedures each year! Why are we so busy? Because we are home to some of the best and brightest medical professionals in the world. This deep well of expertise has led us to become a provincial referral centre for patients from across BC and Yukon needing highly-specialized care.
Here are a few of the areas in which we are provincial – and often national and international – leaders in surgery and complex care.
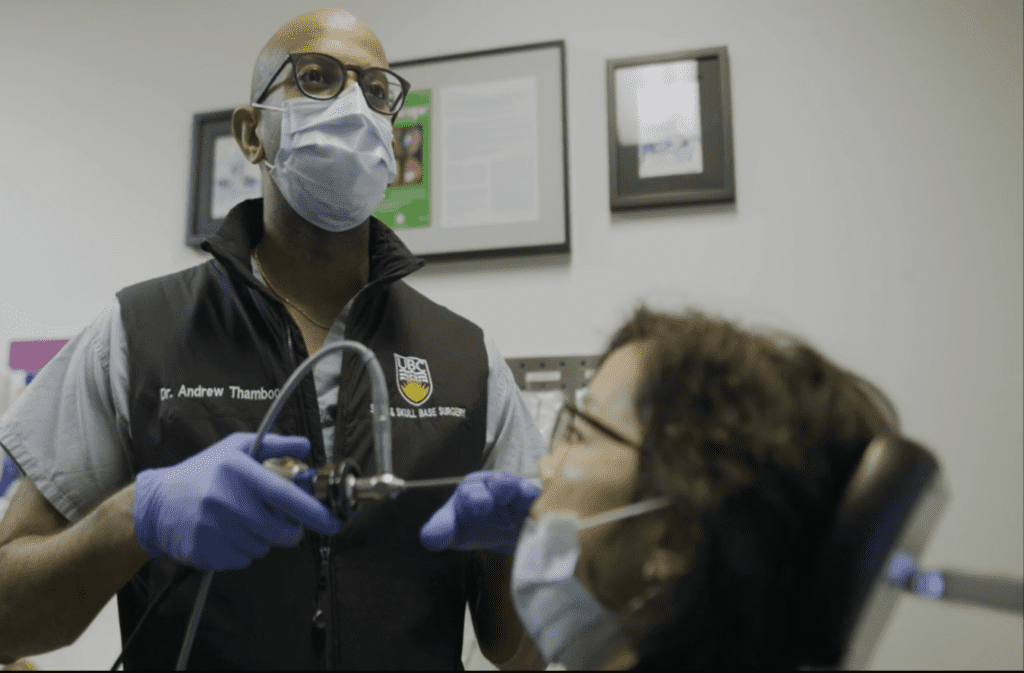
“I’m not just here to add years to your life. I want to improve the quality of your life. So you can speak well, smell the flowers, enjoy your food – all the simple things. ”
Dr. Andrew Thamboo
Rhinologist, Research Director, St. Paul’s Sinus Centre
Your donation supports this life-saving research.
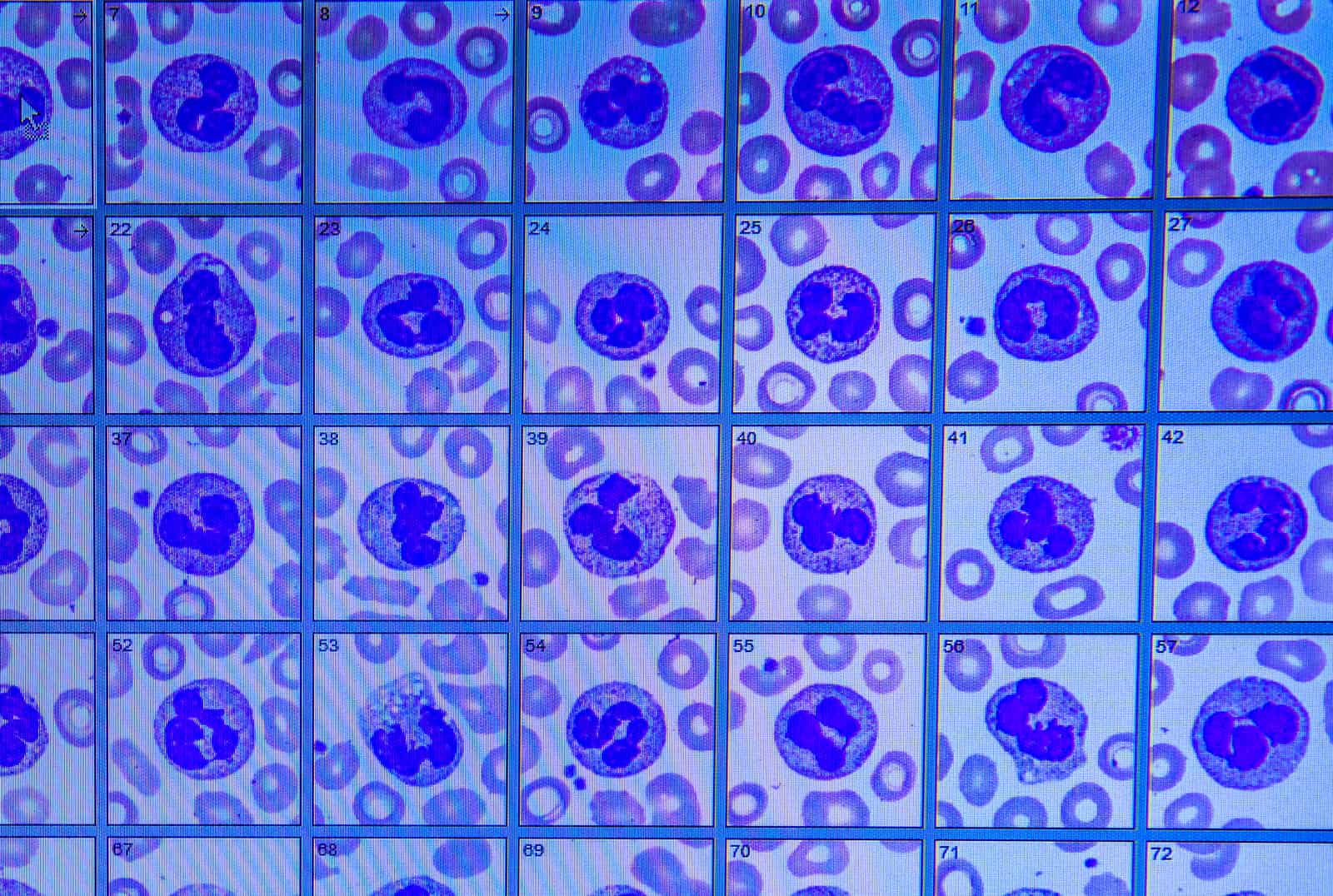
Dr. Thamboo and his team are working with the BC Cancer Agency to identify blood markers for nasopharyngeal cancer that could detect NPC in its earliest stages.
Read more about NPC and how we’re pioneering new, minimally invasive treatments for NPC and other cancers that disproportionately affect Asian Canadians.