Article originally appeared on PHC’s The Daily Scan
Until his recent passing, Dr. Kenneth Forde, a Columbia University Medical Centre surgeon, was a pioneer in promoting colonoscopies as a routine, non-surgical means of detecting early signs of gastrointestinal and colorectal cancer and removing precancerous polyps. Renowned for performing a televised colonoscopy on media personality Katie Couric, his educational legacy lives on as do the many patients who were saved by the cancer screening tool, including Vancouver resident Michael Tresidder.
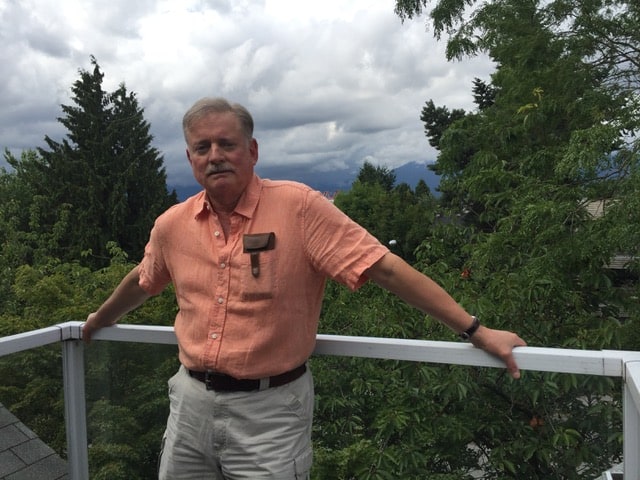
Tresidder, 66, has seen his life come full circle at St. Paul’s Hospital, having been born and recently treated there for a potentially life-threatening disease. After a medical check-up four years ago indicated blood in his stool, his family doctor sent him for his first colonoscopy. Half a dozen polyps were removed and he was scheduled for another procedure in three years’ time. A second colonoscopy performed last April revealed a stage 1 cancerous polyp.
“My family doctor advised me to have regular colonoscopies. I followed her advice which resulted in my cancer being discovered in a timely manner. Without the colonoscopy, the cancer undoubtedly would have spread, leading to a rather grim prognosis,” said Tresidder, a semi-retired respiratory assistant at VGH.
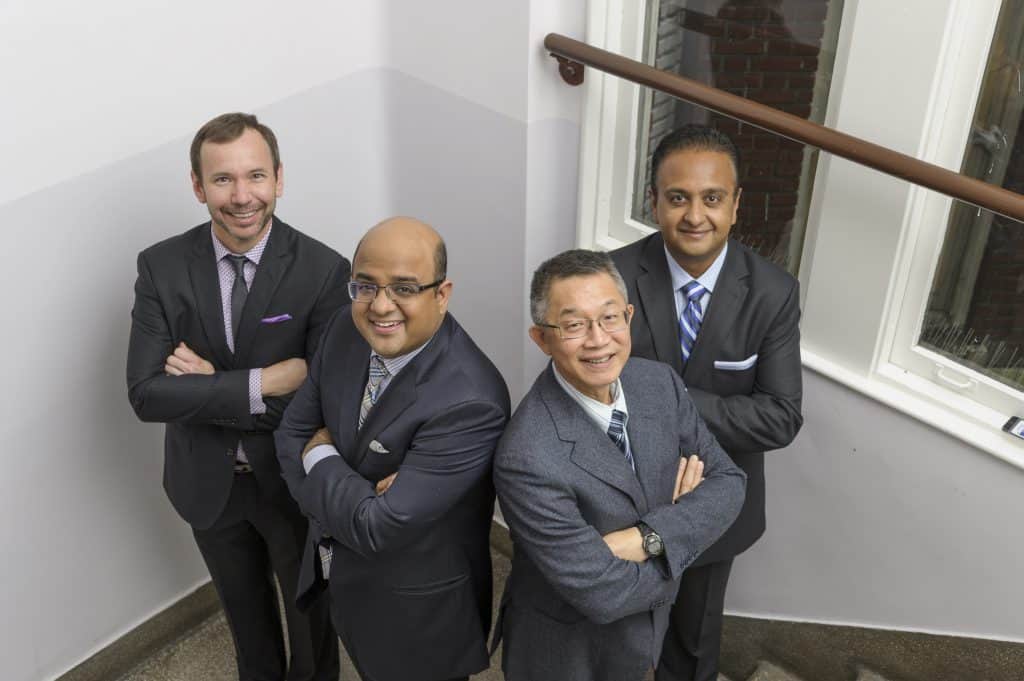
St. Paul’s surgeon says colonoscopies have laser-like accuracy
Dr. Carl Brown, a subspecialist colorectal surgeon at St. Paul’s, concurs with Forde’s message that colonoscopies are an efficacious cancer screening tool. With a miss rate of less than three per cent, colonoscopies are very accurate in diagnosing colon cancer in patients who have the disease. More importantly, having a screening colonoscopy (where polyps can be removed) dramatically reduces one’s chances of dying from colon cancer in the long run.
He adds that the way in which colonoscopies are performed has changed. Previously done with a scope equipped with an eyepiece for visualization, high-definition cameras and scope guidance technology are now used, making polyp detection much better and the procedure much more comfortable.
Why people don’t get tested
Brown admits there are barriers to testing, embarrassment being chief among them.
“People are reluctant to see a doctor if it means they might need a rectal exam or a colonoscopy. There was a great poster campaign a couple of years ago saying don’t die of embarrassment,” says Brown.
However, the greatest misconception is that the procedure will hurt.
“Everyone gets a little cramping, but the combination of sedation and a skilled endoscopist minimizes this issue. Most patients are surprised after the procedure that it was so straightforward,” adds Brown.
FIT test not always the right fit
For patients 50 and older who do not have symptoms (rectal bleeding, change in bowel habit), a fecal immunochemical test (FIT) that checks for microscopic blood in the stool is the recommended screening tool. According to Brown, a FIT test is the best way to avoid colonoscopy in patients with a low risk of having an advanced polyp or cancer. If a FIT test is negative, there is a very low risk of a cancer. FIT tests enable health care providers to ensure that colonoscopies are reserved for the patients who would benefit from them the most.
However, Brown emphasizes that a FIT test is not an appropriate diagnostic tool for patients who see blood in their stool or on toilet paper. He urges them to meet with their family doctor as soon as possible to discuss colon cancer screening. Similarly, if someone experiences significant change persisting beyond one day in the calibre, frequency or texture of the stool, it should be evaluated.
“People with these symptoms should not have a FIT test – these symptoms suggest a colonoscopy is warranted in most people,” says Brown.
Last year, St. Paul’s performed 8,130 colonoscopies and Mount Saint Joseph Hospital 1,970.
Colorectal cancer is the second most common cancer in Canada with 94 per cent of colorectal cancers occurring in adults 50 and over. Risk factors are age, physical inactivity, smoking, heavy drinking, overweight or obesity, diet high in processed meat or red meat, family history of colorectal cancer, and colorectal polyps or inflammatory bowel disease (IBD). Regular screening for colorectal cancer is recommended for average risk adults aged 50 to 74.
Your gift will help further research into diagnosing and testing of colorectal cancer, and continue to support St. Paul’s which has become the colorectal referral centre for patients across BC and, in some cases, Western Canada. Give now.