Published Promise 2018
Research hospitals like St. Paul’s depend on grants from provincial, national, and even international sources. The competition for these resources is fierce, as is the prestige of winning them. So when Providence Health Care heart and lung researchers swept the last round of Canadian Institutes of Health Research (CIHR) grants – garnering awards for eight projects worth more than $6.5 million – the achievement was well noted.
“One can see it as the federal government granting agencies putting a seal of approval on St. Paul’s as the primary centre for heart and lung research in Canada,” says Dr. Don Sin, director of the Centre for Heart Lung Innovation (HLI) at St. Paul’s Hospital. “In COPD [chronic obstructive pulmonary disease] research, we are number one in Canada and top-three in the world, something we should really be proud of.”
Over 140,000 BC residents are currently living with COPD, an incurable, progressive condition that affects breathing (previously called emphysema or chronic bronchitis). COPD is a leading cause of death and hospital admissions across Canada and is the third leading cause of death worldwide.
St. Paul’s designation as a global centre for COPD research is duly deserved; a recent ground-breaking discovery led by Dr. Tillie-Louise Hackett, principal investigator and associate director at HLI, is set to change how COPD patient care is managed in Canada and the world. Hackett has discovered that patients diagnosed with mild and moderate COPD have already lost up to 50 per cent of their small airways.
“Over the last 20 years, there have been hundreds of well powered, well financed clinical trials in COPD, but we were looking in the wrong place as they included severe COPD patients,” says Hackett, whose continuing studies were awarded $675,000 in the last round of CIHR funding.
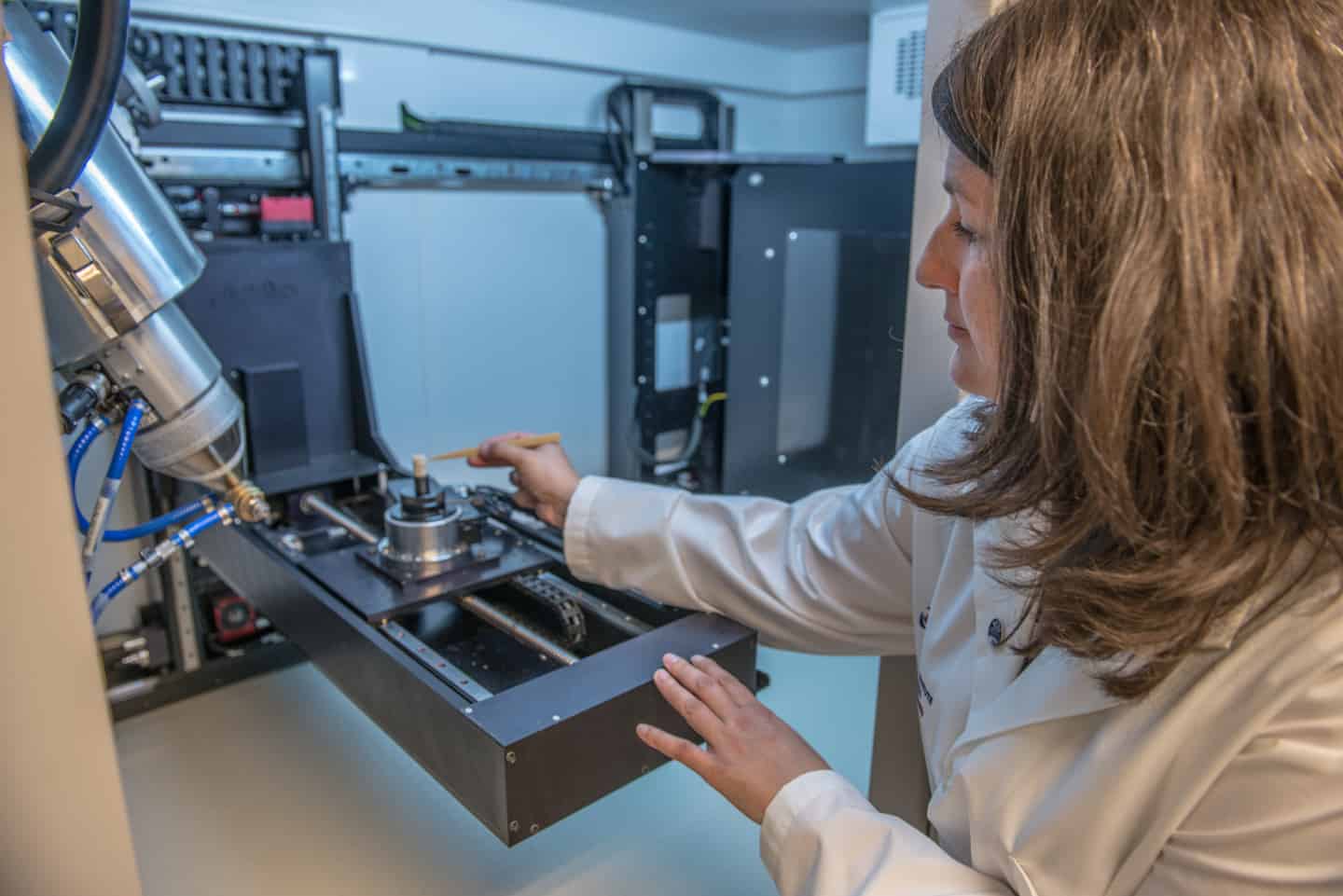
Using a high-resolution micro-CT scanner, one of only three such machines in Canada, Hackett was able to unlock the full potential of St. Paul’s globally renowned tissue bank (one of the largest lung tissue repositories in the world) and provide evidence of substantial lung damage before symptoms arise.
“I was very lucky that HLI not only had a Canadian Foundation for Innovation (CFI) award for infrastructure, but also that St. Paul’s Foundation partnered on that award,” says Hackett. “Without their funding, we would not have the micro-CT scanner, and without that scanner, I could not have performed the important experiment in the published study.”
“To be honest, without the largesse of the Foundation and its various donors a lot of these opportunities would be lost to us,” says Sin. “Many of these fundraising opportunities require matching funds and the Foundation has been very helpful in putting up those partnering funds.”
“And it’s not just one-to-one matching,” he continues. “Let’s say that there’s a $100,000 investment by the Foundation. It can be amplified into a $1-million investment by external organizations. We call it synergy at the scientific level, tremendous synergy.”
Earlier this year, the ever-growing HLI won its fourth straight CFI infrastructure award, worth over $6 million, with a portion earmarked for the purchase of a mass spectrometry system and 3T MRI machine, the only one of its kind in Western Canada dedicated for heart and lung research.
St. Paul’s heart and lung researchers have even more recently obtained five new provincial grants from the Michael Smith Foundation for Health Research to attract and retain the best and brightest young scientists to the Centre.
“The Centre for Heart Lung Innovation has become an ecosystem of funding, and it has created this critical mass of expertise,” says Cecilia Tupper, director of major gifts at St. Paul’s Foundation. “It’s not an easy thing to sustain, but St. Paul’s is doing it.”
Another principal investigator at the Centre, Dr. Pat Camp, won $1,595,025 from two research grants submitted in the last round of CIHR awards. Her research focuses on the problem of COPD in native communities in BC’s north. Camp aims to improve these communities’ access to treatment by implementing rehabilitation programs outside the hospital setting and piloting telehealth strategies and wearable devices to reach lung patients living in remote areas.
HLI researchers are also solving complex transplant problems. Drs. Bruce McManus, Raymond Ng, and Scott Tebbutt received a $2.2 million CIHR grant (one of the biggest in history) to develop novel blood tests to detect heart rejection in transplant patients before a complete heart failure. This test will enable doctors to treat the rejection before it’s too late, preventing repeat transplantation and even death.
The benefits of the work being done at St. Paul’s are felt far beyond the city limits, changing the lives of patients across BC, Canada, and the world.
You can help support the life-changing work being done by donating today at donate.helpstpauls.com/HLI.
Photography by Jeff Topham | Graphic by Irvin Cheung