Published Promise 2018
Thanks to revolutionary research done at St. Paul’s, patients suffering from chronic rhinosinusitis (CRS), a complex disease that affects not only the nose and sinuses but also has broad negative effects throughout the body, can potentially be cured.
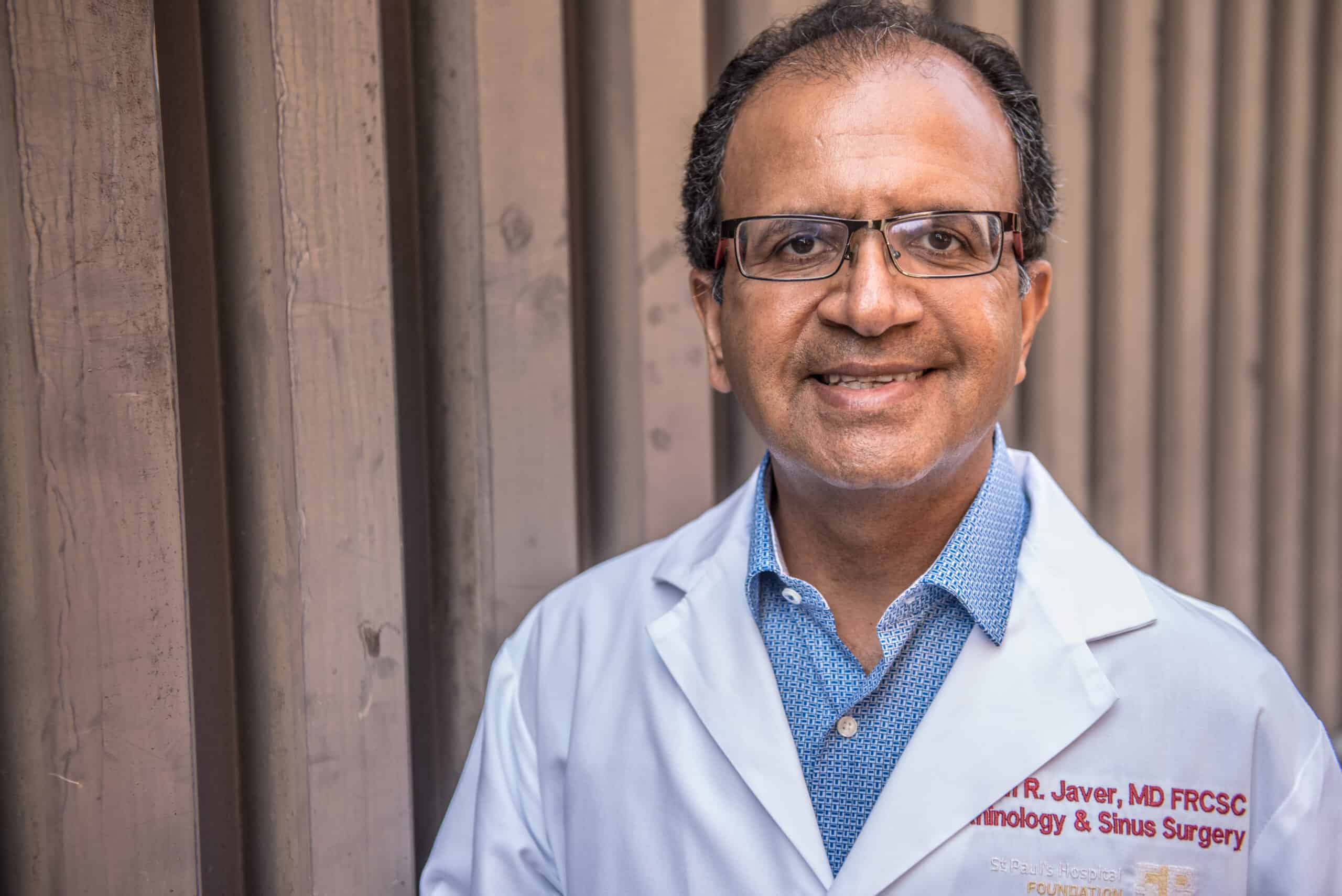
According to Dr. Amin Javer, sinus surgeon and director of St. Paul’s Sinus Centre, CRS affects a large section of the population, yet there is little awareness about this patient population and how much they suffer. “Of the 12 per cent of North Americans who suffer from CRS, 25 per cent of those patients currently can’t be helped with any medical or surgical intervention,” he says, adding there are more people suffering from sinus conditions than diabetes. “That’s a huge number of people with debilitating daily symptoms that greatly reduce their quality of life.”
As a world leader in CRS research, Javer has dedicated his career to helping patients who struggle daily with chronic infections, ones that currently have no treatment options. His years of groundbreaking research have culminated in a new treatment which has never been attempted before: a sino-nasal microbiota transplant (SNMT).
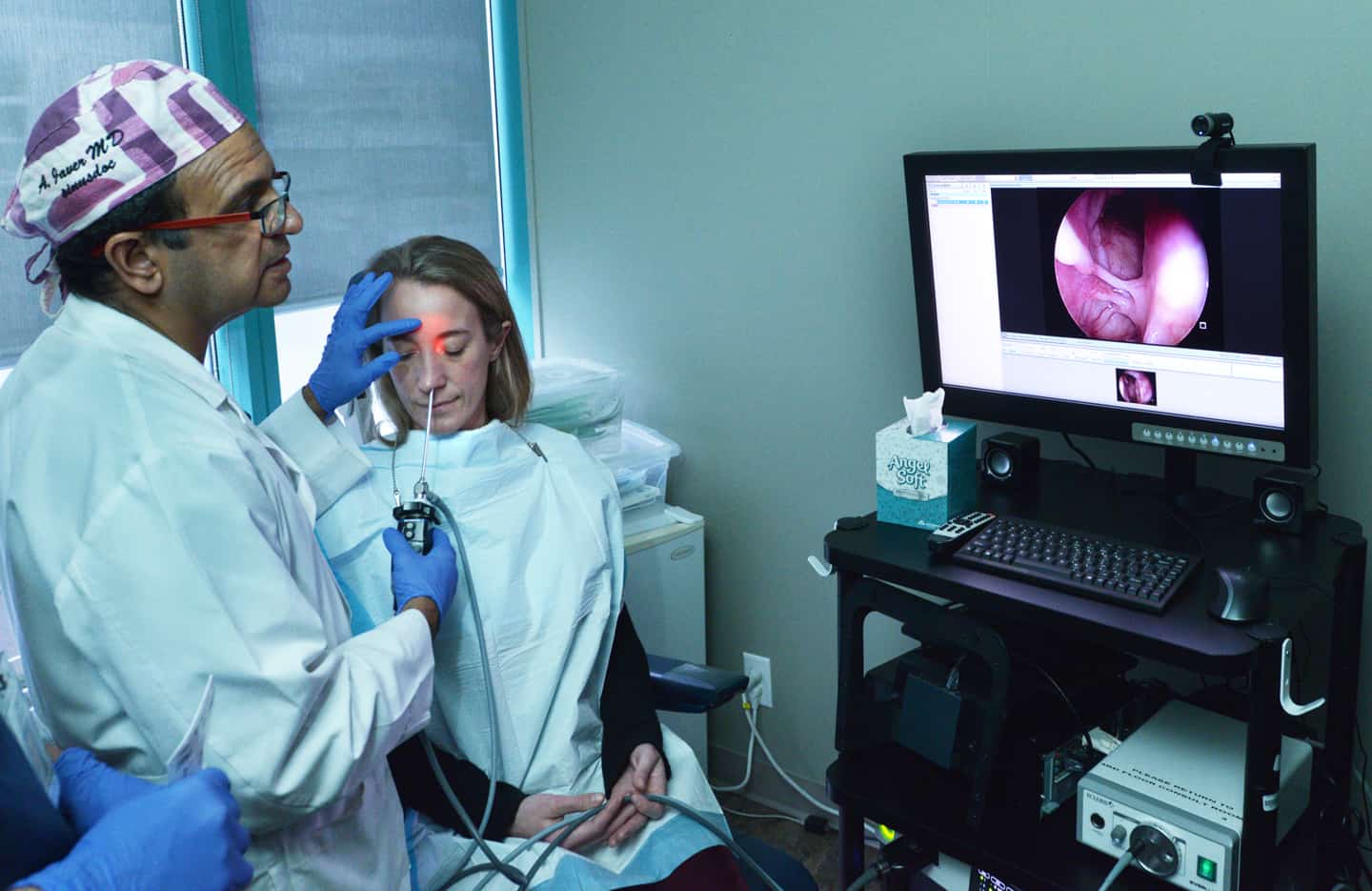
SNMT begins with a primary treatment of antimicrobial Photodynamic Therapy (aPDT), a process which sterilizes the sinuses and kills all bacteria, and then involves taking nasal mucus – snot – from a healthy nasal cavity, treating it, and then transplanting it into the CRS patient’s affected sinus(es) over three sessions of treatment. The patient is then examined again after one, two, three, six and 12 months, and doctors test the results to gauge SNMT’s effectiveness over time. This innovative procedure has the potential to cure this painful, lingering and, up until now, untreatable condition.
“We have patients who come in every week and every treatment has failed them. I wanted to help. So I started to look at different options; I started looking at anti-microbial treatments that haven’t been used in the nasal cavity before,” Javer says.
Javer investigated and tested different methods but none of them provided a permanent fix. That was until he started thinking about injecting snot from donors with healthy sino-nasal bacteria in an attempt to change the overall microbiome in the diseased sinus, similar to recent fecal transplants that have done the same for those with inflammatory bowel disease. More than 90 per cent of fecal transplant patients see positive results.
The risks from SNMT appear to be minor, such as cold-like symptoms that may last a few days, but SNMT’s potential to cure patients from a host of daily challenges is huge. CRS patients commonly deal with excessive coughing, nasal blockage and congestion, nasal discharge, post-nasal drip, facial pressures and headaches, sinus infection and inflammation, and more. In addition, sufferers report feeling fatigued and lacking mental clarity and concentration because they have very poor sleep quality. These patients can also experience a decrease or loss of sense of smell and taste, resulting in a loss of joy from simple pleasures like savouring a delicious meal.
Another devastating effect of CRS is that, all too often, family members don’t see their loved one’s disease as a serious problem. “CRS is a chronic disease that’s hidden in your sinuses, and patients’ spouses, children and parents will never know how badly you feel,” says Javer. “To them, it’s just your nose: blow it and keep moving.”
It is precisely for this reason that many patients suffer in silence. The impact of this disease cannot be overstated. “I’ve seen a lot of divorces and family breakups because family members just don’t understand how serious this disease is,” adds Javer. “If successful, SNMT will be a game changer in patient care.”
The procedure has been submitted to Providence Health Care’s Research Ethics Board and is awaiting approval from Health Canada later this year.
Photography by Jeff Topham, Dominic Schaefer