Published Promise 2019
Life-saving research has long been part of the history of Providence Health Care (PHC). The first steps to formalize the process date back to 1956, when St. Paul’s departments of medicine, pathology, and surgery joined forces. Together, they established the Clinical Investigative Unit and launched the hospital on a path to becoming an influential research and teaching hub.
The BC Pulmonary Research Lab opened in 1977 and marked St. Paul’s first step into significant laboratory research. The hospital recruited a dream team from McGill University: Dr. James Hogg and Dr. Peter Paré. The pair went on to make enormous contributions in lung research. In particular, their work on asthma and COPD catapulted St. Paul’s to the forefront of global research.
PHC expanded into cardiovascular research with the arrival of Dr. Bruce McManus, an internationally known cardiac pathologist, in the 1990s. Being located in the hospital was an incredible bonus for researchers, giving them easy access to other researchers, scientists, and most importantly, patients. Set in this environment, research staff could easily translate newly acquired academic knowledge into real life changes in practice, patient care, and policy.
In 2005, all PHC research became coordinated through the Providence Health Care Research Institute (PHCRI). What’s unique about PHCRI is its incredibly broad scope across more than 30 departments including heart, lung, and kidney diseases, HIV/AIDS, mental and urban health, addiction, and aging.
Life-or-death research in the ER
In 2010, a patient arrived at St. Paul’s Hospital in cardiac arrest. A young, previously healthy mother, she was suffering from acute myocarditis (an inflammation of the heart) and had been receiving CPR for nearly two hours. Despite what looked like a dismal chance of survival, physicians weren’t ready to give up. Cardiovascular surgeon Dr. Anson Cheung put her on an ECMO (Extracorporeal Membrane Oxygenation) device – a machine that takes over the work of the heart to pump oxygen through the body. Three days later, she woke up asking, “What’s going on?”
Her road to recovery was tough, but today that patient is thriving. “She goes to the gym five days a week. She’s a normal mom,” says Dr. Jim Christenson, head of the UBC Department of Emergency Medicine and executive lead of the BC Emergency Medicine Network, which connects practitioners across 108 emergency departments to share knowledge and resources.
The dramatic experience with that young patient inspired Christenson and his colleague Dr. Brian Grunau, in collaboration with St. Paul’s Heart Centre, to develop a clinical program to research whether patients with out-of-hospital cardiac arrest who fail all standard treatments could be revived with ECMO. Incredibly, they’re finding that for certain patients, recovery is indeed possible.

With that knowledge, the Emergency Department implemented an ECPR simulation program – the first in Canada – to help keep physicians’ skills fresh so they can quickly respond to patients needing ECMO.
Christenson has been researching cardiac arrest for decades and runs a provincial research unit looking at the best methods to resuscitate cardiac arrests. Thanks to this research unit, BC now boasts a 16 percent survival rate for sudden cardiac death, one of the highest in the world.
“By improving overall survival from six to 16 percent over the past 10 years, we have an extra 200 survivors per year in BC,” Grunau points out. “If we could bump that up to 25 percent, we would have an additional 200 survivors per year.”
St. Paul’s emergency team has produced landmark research in other areas too, and these findings have set many standards of care in the emergency room, including how soon to safely discharge overdose patients and patients with chest pain, and how long to attempt resuscitation in different scenarios.

The science of miracles
St. Paul’s own Dr. Julio Montaner is an internationally renowned clinician and scientist whose groundbreaking research has curbed HIV/AIDS around the world. Throughout the 1980s and ’90s, Montaner researched antiretroviral therapy strategies to develop what we now call highly active antiretroviral therapy (HAART). The treatment is nothing short of miraculous: it suppresses HIV replication, promotes immune recovery and remission, and can stop HIV transmission. It has become the global standard of care endorsed by both the UN and the WHO. Montaner also pioneered the innovative Treatment as Prevention®, further driving down new cases of HIV and, in tandem with sustained treatment, preventing HIV transmission.
Cardiac innovation is another area of rare distinction at St. Paul’s. To cite just one example, Dr. John Webb’s life-changing heart valve surgery. Called one of the “most exciting events in cardiology in the last 50 years,” Transcatheter Aortic Valve Implantation (TAVI) gives hope to patients who are too ill for open heart surgery. With it, the new valve is tucked inside a narrow catheter and threaded up to the heart through a tiny incision in the groin. Since Webb pioneered it in 2005, TAVI has improved the lives of more than 350,000 people in over 40 countries. Thanks to generous donors, St. Paul’s has a virtual teaching lab that streams TAVI procedures to train doctors around the world.
Putting patients first
Patients are at the centre of a bold new project for kidney care under the leadership of Dr. Adeera Levin, head of the UBC Division of Nephrology at St. Paul’s. In 2016, Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease Network (Can-SOLVE CKD) was launched with $40 million in funding through the Canadian Institutes of Health Research and $1 million from donors to St. Paul’s Foundation.
This five-year program engages patients as partners to investigate the value of early screening, patient education, new drug treatments, and stem cell therapies. The goal is to learn directly from patients what does and doesn’t work for them, and to use that feedback to improve care for all.
“The patients involved in this research are active participants, not just as tissue donors,” explains Dr. Darryl Knight, new vice-president of Research and Academic Affairs for PHC.
He cites St. Paul’s recently established Scleroderma Clinic as another example of research in partnership with patients. Scleroderma is a progressive autoimmune disease that causes tough, scar-like tissue to build up in the skin. In turn, this weakens blood vessels, damages organs, and affects breathing. There is no cure. At least, not yet.
But there’s a lot of hope surrounding a leading-edge “proof of concept” genome study of scleroderma biomarkers. It’s a mouthful, but it means measuring the specific biological components of each patient’s disease – markers which are different for everyone – then developing a treatment specifically tailored to those characteristics. “It’s personalized medicine – adapting the therapy as we learn how each patient responds,” says Knight.
The future of research
Today, with the support of donations to St. Paul’s Foundation, PHC continues to leverage emerging technologies as a founding member in Canada’s Digital Technology Supercluster. Basically, the Supercluster fast-tracks innovation by building partnerships, pooling resources and data, and facilitating projects beyond the reach of any single organization.
Our first project is a new diagnostic tool that will help save and improve the lives of people with skin cancer, a disease where successful treatment is critically dependent on early detection. It’s called the Intelligent Dermatology Network. Here’s how it works: a doctor in Fort St. John uses her cell phone to submit photos of a patient’s suspicious mole to a cloud-based network fortified with artificial intelligence. With thousands of pictures in the network and more being uploaded all the time, it “learns” to distinguish between cancerous and benign moles. The anxious patient doesn’t have to wait for a specialist, travel to a major health centre, or take time off work. Most importantly, a fast, accurate diagnosis means treatment can begin right away.
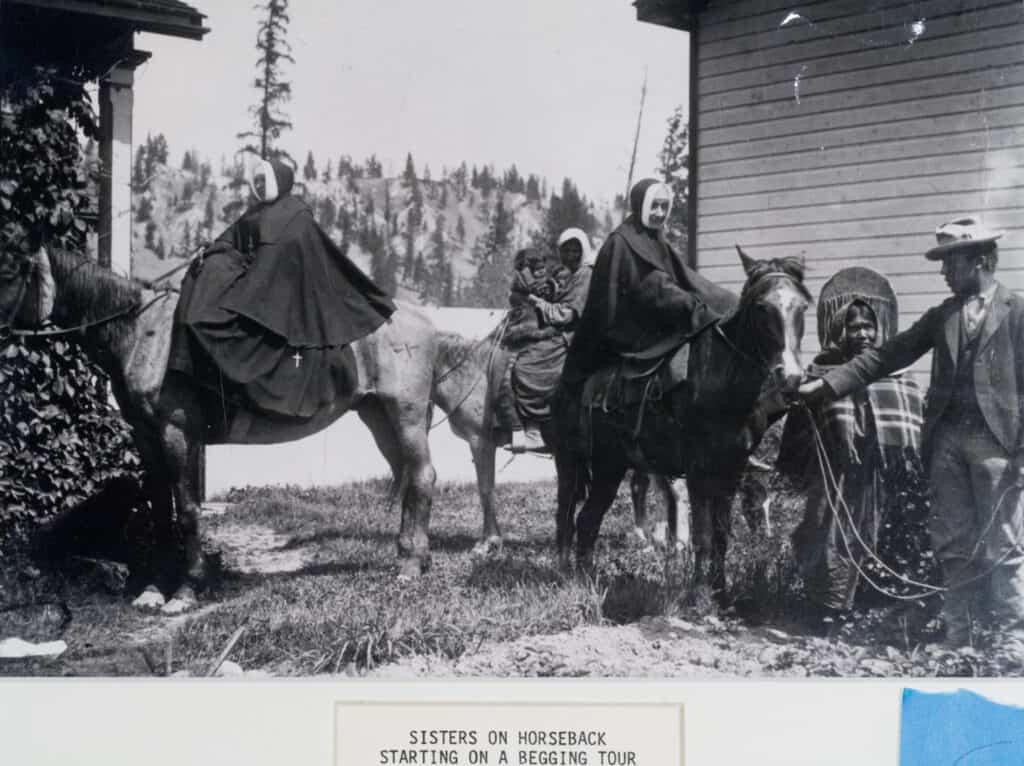
From bench to bedside, PHC doesn’t just embrace change, we drive it. After all, we are BC’s original health science innovators and have been since 1918 when Sister Spinola engineered an ether-warming machine to stop patients from going into shock. This kind of initiative will only increase when we move into the new St. Paul’s: a state-of-the-art hospital and life sciences campus specifically designed to facilitate research, discoveries, and of course, compassion.
Help support the next 125 years of research at St. Paul’s. Donate now.