Published Promise 2019
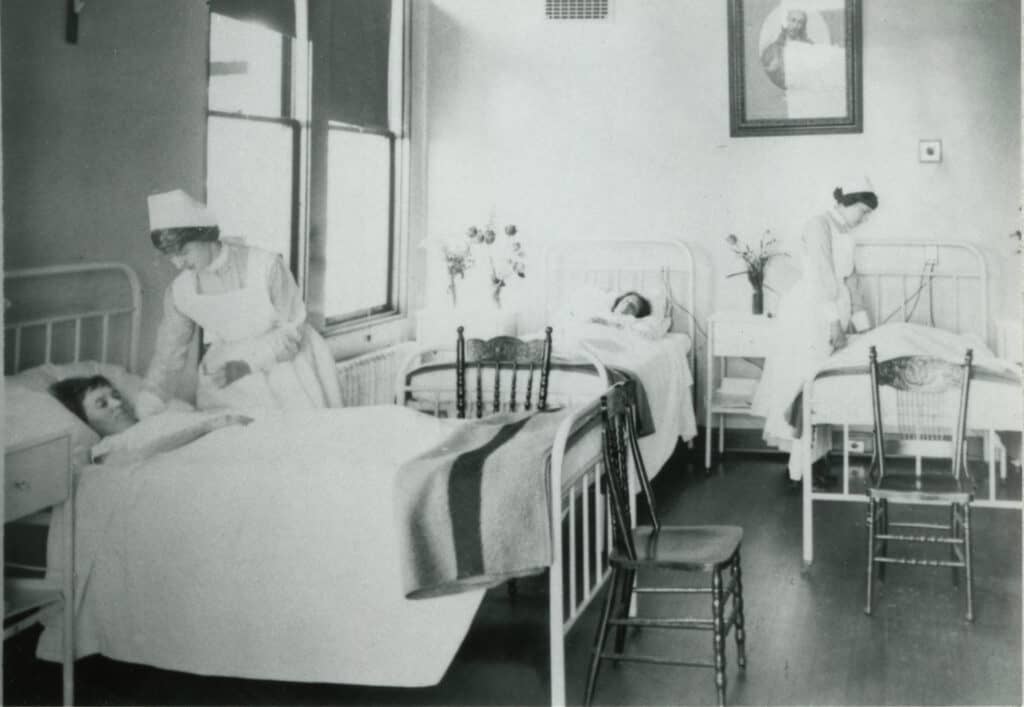
Almost from its very beginning, St. Paul’s has been a teaching hospital. In 1900, the hospital’s seven nursing nuns cared for 561 patients. It was a scramble to keep up and by 1907, they were desperate for help. So they boldly decided to open a nursing school – recruiting from outside the convent for the very first time. A call went out to women over 20 years of age, of good character, and in good health. That same fall, 14 women pledged to uphold the school’s motto, “Enter to learn, go forth and do good.”
That initial class, and the Sisters and physicians who trained them, were trailblazers setting a course for 125 years of teaching excellence at St. Paul’s. And they were the first in a long line of nurses, interns, residents, fellows, and physicians to establish the hospital’s world-renowned culture of “paying knowledge forward.”

Training for nurses back then was basic: beds, baths, and bandages. Expected to obediently and unquestioningly follow doctors’ orders, the role of nurse was subordinate. After earning respect in World War I, and then again in World War II, nurses proved themselves invaluable and thus, a team approach between nurses and doctors was born.
Hands-on med school
St. Paul’s overcame a dearth of doctors in its early years the same way it did the nursing shortage, by training in-house. Two interns (Dr. Rush during the day, and Dr. Zito at night) joined in 1928. Early on, it was decided that the interns should be paid. This radical idea gave St. Paul’s a distinct advantage in recruiting the most promising young doctors. By 1952, the wards were teeming with medical students; St. Paul’s was now officially a teaching hospital.
In 1992, to fix a province-wide doctor shortage (and overcome the difficulty internationally-trained doctors had establishing themselves in Canada, often due to accreditation obstacles), St. Paul’s launched the International Medical Graduates Program, offering residencies to international MDs. In its first 14 years, it helped 52 graduates – many with in-demand, second-language skills – earn their licences and increase the number of physicians in BC.
Specialized expertise
Over the years, St. Paul’s has asserted itself as a global leader in specialty training. Dr. William Ross, clinical professor of ophthalmology at UBC, trained stateside at Wills Eye Hospital in Philadelphia. After returning to Canada and establishing the vitreoretinal service at St. Paul’s, Ross took on his first fellow in 1986. He has since trained 57 vitreoretinal surgeons, more than half of whom have come from the States.
“The fact that Americans come up to St. Paul’s speaks highly about how well recognized our fellowship is,” says Ross. “Every year we get 65 to 70 applications from all over the world for our two positions.”

Ross is working hard to keep up with that demand. In addition to having trained some 120 UBC residents over his 45-year career, he oversees another fellowship, this one established with a $1.375-million donation by former oil patch CEO Gwyn Morgan, whose eyesight was saved by Ross. Moved by this generosity, Ross invested $1.34 million of his own money into a third fellowship, which provides post-residency training for ophthalmologists in developing countries.
At 76, Ross says, “I never want to stop teaching. It gives me the greatest satisfaction to pass on my skills, my knowledge, and my judgment.” He’s currently launching a new teaching fellowship program (courtesy of a recent gift by another grateful patient, Mr. Shirvan Bakhtiyari, who donated $600,000), which will support the training of medical retina specialists for the next 11 years, well into the tenure of the new St. Paul’s.
Educating, and learning from, the next generation
“In the past, we would all leave the country to train elsewhere because Canada just didn’t have fellowships,” says Dr. Amin Javer, director of St. Paul’s Sinus Centre, who left Vancouver to train in the US. Wooed by his American mentor, Dr. Frederick Kuhn, he almost didn’t return.
“I would not have come back to Vancouver if it wasn’t for St. Paul’s,” says Javer. He credits St. Paul’s Foundation with helping to realize his dream of setting up a world-renowned sinus and skull-based surgery training institute. Javer’s teaching has gone beyond BC’s borders. “I’ve made it a mission to train fellows from countries where they would have the greatest impact,” he says. His first fellow, in 2002, was from Singapore and is now “running the show” back home. The same goes for his former pupils in Mexico and Chile. “My fellow in Saudi Arabia has become the chairman of the department. My fellow in the UK is now a full professor,” he says.

It’s a win-win relationship, Javer adds. Welcoming young doctors, “brings in new ideas, new research. It keeps us on the cutting edge.” Those rewards are passed on to patients, he says, noting that his efficiency would drop by 25 percent without the help of his fellows. As for the international recognition his research has received for major breakthroughs in rhinology, it wouldn’t be possible without his fellows: “I would just not have the time.”
Javer, now up to three fellows a year, also has aspirations for the new St. Paul’s. “We can have more fellows, we can do more research. I just see a trajectory that is going to take us much, much higher,” he says.
Nursing never more valued
Education at St. Paul’s has experienced a remarkable trajectory: from 14 nursing students in 1907 to one of Canada’s most sought-after internship programs today. “Nurses are uniquely valued at Providence and that’s translated into so many education, research, and teaching opportunities,” says Sandra Lauck, PhD, citing her own pioneering professorship in cardiovascular nursing.
The first professorship of its kind in Canada, her role “bridges the university and clinical practice,” says Lauck. “Rather than staying in an office up on the hill, I’m down here in the cardiac program close to the patients and the clinicians, with my finger on the pulse of the issues that matter most.”
“Empowering nurses directly results in better patient care,” says Lauck. “Nurses have more contact hours with patients than any other health care professional.” One of the ways she’s doing this is by encouraging nurses to gain research expertise and change nursing practice through the PHC Practice-Based Research Challenge. This is an annual competition where nurses work with mentors to design and implement research projects that lead to practice changes and improvements. Guiding the next generation is the cornerstone of Lauck’s professorship. “I owe my own career to the collective mentorship of multiple nurses at St. Paul’s,” she says.
As for what the new St. Paul’s has in store for nursing, Lauck has some ideas. “I’d like this nursing professorship not to be an anomaly or something unique, but rather an expectation. So that across the board – in mental health, or palliative care, or general surgery – we strengthen the role that nurses play as clinician scientists to ensure that nursing at St. Paul’s stays at the forefront and contributes to multidisciplinary innovation.”
Help support the next 125 years of teaching at St. Paul’s. Donate now.