Published Promise 2023
Kathy Deyell spent three years caring for her elderly mother. Tired and busy, it never occurred to her that something might be wrong inside her own body.
“While I was caring for mom, I didn’t take the time to care for myself,” says Deyell. “Before I knew it, I was three years behind on my mammogram.”
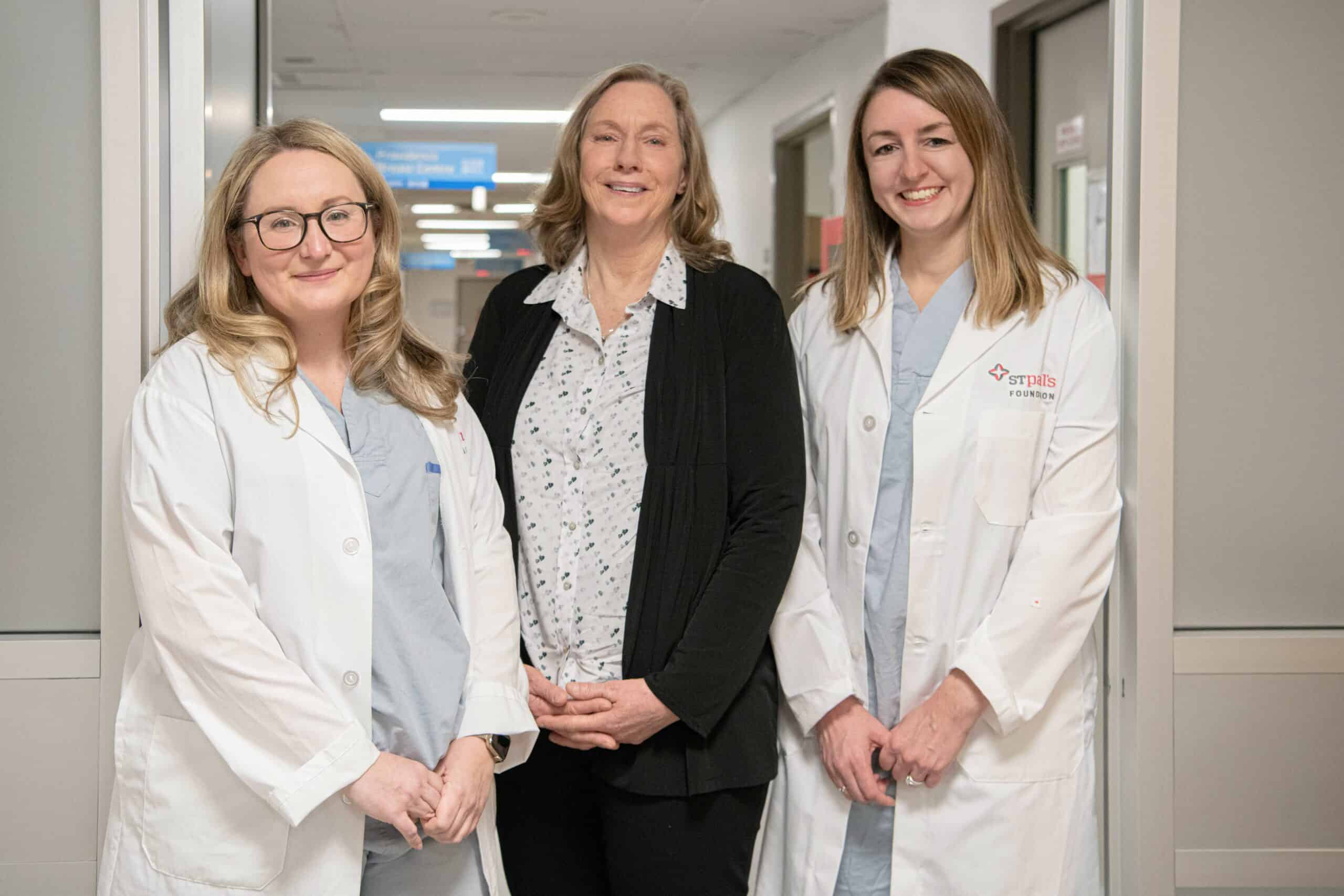
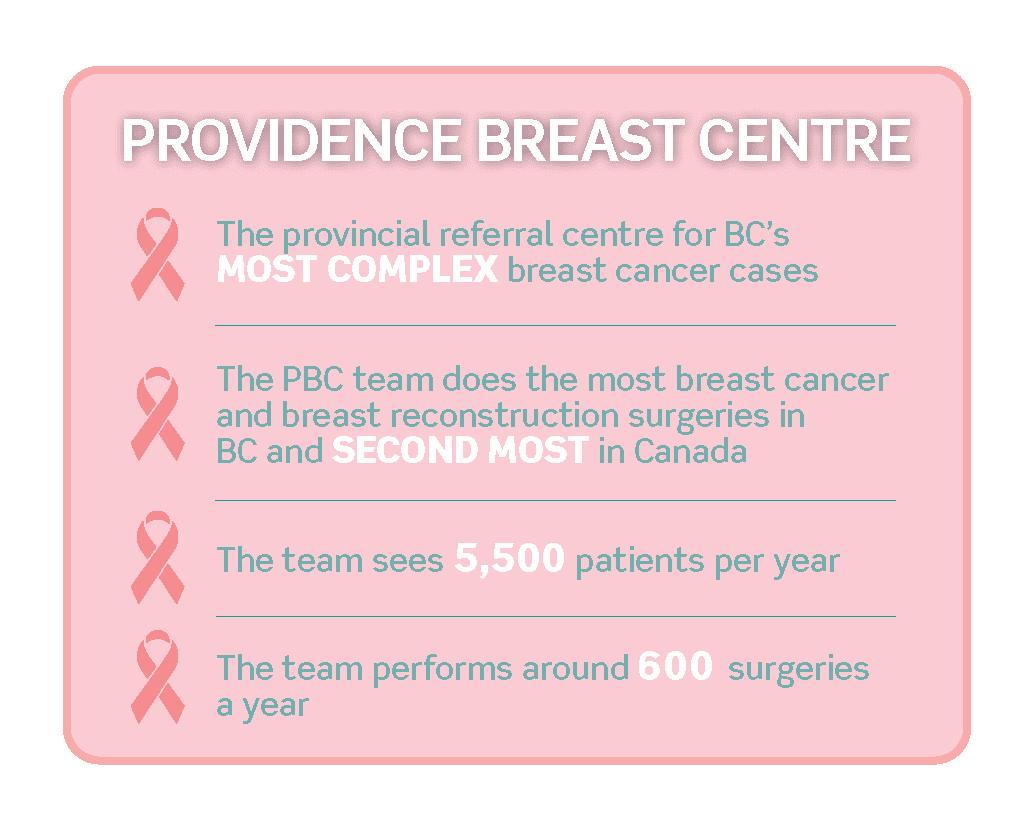
In 2021, she finally went for a screening mammogram. A follow-up ultrasound and biopsy confirmed her worst fear: she had stage one breast cancer. Her GP explained that surgery would be her best option and she referred Deyell to Dr. Amy Bazzarelli with the Providence Breast Centre (PBC) at Mount Saint Joseph Hospital.
“Dr. Bazzarelli gave me two options,” recalls Deyell. “I could have a guide wire inserted or take part in a trial for the Breast Centre Seed Localization Program [using the MOLLI system].”
The Breast Centre Seed Localization Program (BCSLP) is the “eureka moment” – or rather, the eureka magnet – that helps surgeons more easily locate and remove cancerous tumours.
Deyell jumped at the chance to participate and became PBC’s 12th BCSLP patient. Ten days before her surgery, she had a tiny magnet placed deep into her breast to mark the tumour site. “It was easy and painless,” Deyell says. “No worse than a minor dental procedure.”
Kinder. Gentler. More accurate.
MOLLI stands for Magnetic Occult Lesion Localization and Imaging. It’s a long name for a simple-yet-sophisticated innovation pioneered at Toronto’s Sunnybrook Health Sciences Centre.
Tumours deep in the breast tissue, and those that aren’t palpable, can be hard for surgeons to find and fully remove.
“Before BCSLP, a radiologist would place a wire into the breast,” Dr. Rebecca Warburton, head of PBC, explains. “The surgeon would then follow the wire to the tumour.”
Unfortunately, the wires would often move around. “Obviously, that’s painful for the patient. It’s also much more difficult for the surgeon to pinpoint the lesion,” says Dr. Warburton.
With MOLLI, the radiologist uses a mammogram or ultrasound to guide a small needle to the tumour to implant the magnetic seed. Unlike a wire, which needs to be placed in the patient the day of the surgery, the seed can be put in place up to 30 days before, streamlining the process significantly.
Once in the OR, the surgeon uses a wand that functions exactly like a handheld metal detector. The wand picks up the magnetic signal from the seed, and sends images and sounds to a screen or tablet that guides the surgeon to the tumour’s exact location. The cancerous tissue, the margins around it, and the seed itself are then removed safely and precisely.
Dr. Bazzarelli and the PBC team studied MOLLI extensively before the pilot and they were confident that it would vastly improve patient care. “And that’s exactly what happened,” Dr. Bazzarelli says.
Breast Centre Seed Localization Program: Win, win
BCSLP offers so many advantages over the old wire system that it’s fast becoming the new gold standard in care.
“Patients who’ve had both wires and magnetic seeds tell us that their overall care and experience is significantly better with the seeds,” says Dr. Bazzarelli. “There’s less discomfort, much less angst, and there’s less time waiting for their OR to start because they don’t need to have the seeds placed on the same date.”
Dr. Warburton is equally enthusiastic.
Before this technology, radiologists could only perform five wire insertions a day. But, with the seeds, there are no limitations on the number of localization procedures that can happen in a day. Everything is so much more efficient now.
– Dr. Rebecca Warburton
MOLLI has also proven to be more accurate in directing surgeons to the exact location of a tumour. You don’t have to have cancer to appreciate the relief and peace of mind this news brings to patients and their families.
Healing with innovation and compassion
The MOLLI pilot was fully funded by our generous donors and it’s a powerful example of how donor support directly improves patient care.
“We’re proud of our track record and we’re beyond appreciative to the donors who make it possible to bring innovation and compassion to patient care,” says Dr. Bazzarelli.
Deyell is equally grateful. “I’m so thankful I got to participate in the MOLLI study. I felt like I was more than a patient. I was part of the solution!”
These leading-edge innovations will become even more possible with the new Clinical Support and Research Centre (CSRC). Connected to the new St. Paul’s Hospital on the Jim Pattison Medical Campus by sky bridge, the CSRC will expedite collaboration between patients, researchers, clinicians, and industry partners. And it’s these interactions that will spark a transformative circle of research, discovery, and treatment, and lead to the next century of compassionate care.
Reducing risk for future patients
Now that the BCSLP is fully funded, the PBC team is shifting their focus to women with a genetic disposition for breast cancer who haven’t been diagnosed – yet.
These women have a 70% chance of developing breast cancer and could benefit from receiving a risk reduction mastectomy with the option of reconstruction, before cancer develops. These measures can improve quality of life, prevent the need for therapy, and possibly save lives. To take this essential next step, PBC needs a registered nurse whose complete focus will be on helping these patients.
The BCSLP has already begun transforming care for patients at PBC, and the Breast Cancer Risk-Reduction Program will take this compassionate care even further. Give now at donate.helpstpauls.com/BCSLP.