Published Promise 2024
When Karam Roberts and her partner, Matt Holywell, moved to Vancouver in 2019, they were excited to explore all that the West Coast had to offer: stunning hikes, access to ski hills, and enchanting coves in which to scuba dive.
They didn’t expect that just over a year later, Roberts would be fighting for her life against a rare illness. But through the expert collaboration of a team of doctors, and with the help of equipment funded by donors, St. Paul’s Hospital was able to give Roberts her life back.
Only a few months after their arrival in Canada (Roberts is originally from Wales and her partner is from Australia), Roberts became sick with a battery of symptoms: intense sinus pain, stiff joints, fatigue, weight loss, ears blocked filled with fluid, coughing up blood, and difficulty breathing.
“I’ve never been so ill,” says Roberts. “I couldn’t stand up off the sofa. I was in agony.”
The challenges of receiving health care in the middle of the COVID-19 pandemic combined with her alarming respiratory symptoms created the perfect storm. It was only in December 2020, when a doctor ordered bloodwork at St. Paul’s Hospital, that they realized how dire her situation was – and immediately admitted her.
“And then that’s when the St. Paul’s journey began,” Roberts says.
A double diagnosis
With the help of eight St. Paul’s specialists, doctors were able to diagnose Roberts with granulomatosis with polyangiitis (GPA), a rare autoimmune disease and type of vasculitis. It can cause inflammation of different blood vessels in multiple areas of the body, as well as lasting damage to vital organs and tissues. In Roberts’ case, the problem was primarily in her lungs.
“I was just stunned and upset,” Roberts says of receiving the news. “It can be very serious if not treated urgently. I thought, ‘How on Earth are we going to deal with this?’”
The day after beginning treatment in hospital, Roberts woke up with severe chest pain. She remembers a doctor from internal medicine arriving. Then everything went dark. Roberts had suffered a cardiac arrest. She woke up four days later in the Intensive Care Unit, a St. Paul’s nurse at her side.
“I was just so grateful to be alive. I only survived because that doctor was there and she started to do CPR on me straight away,” says Roberts.
The road back to health with vasculitis

Now Roberts was faced with yet another challenge: recovering from a cardiac arrest while treating her GPA. After seven weeks in hospital, she was transferred to the cardiology ward for a defibrillator implant. But the placement of the device, which is typically installed under the collarbone, proved troublesome. “I really didn’t want it there because I wear a backpack every day. And because I’ve lost so much weight as well, it would protrude quite a lot,” says Roberts.
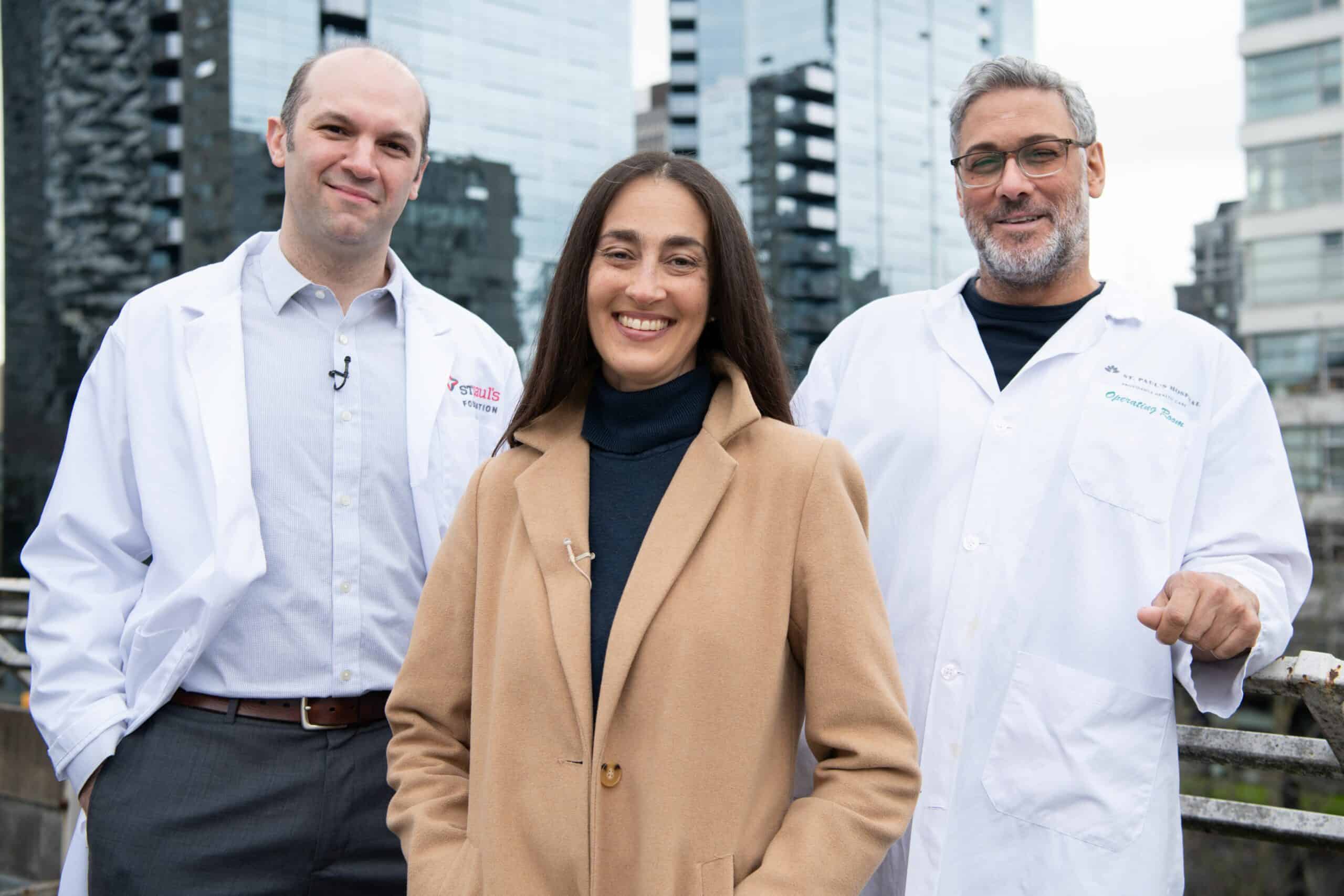
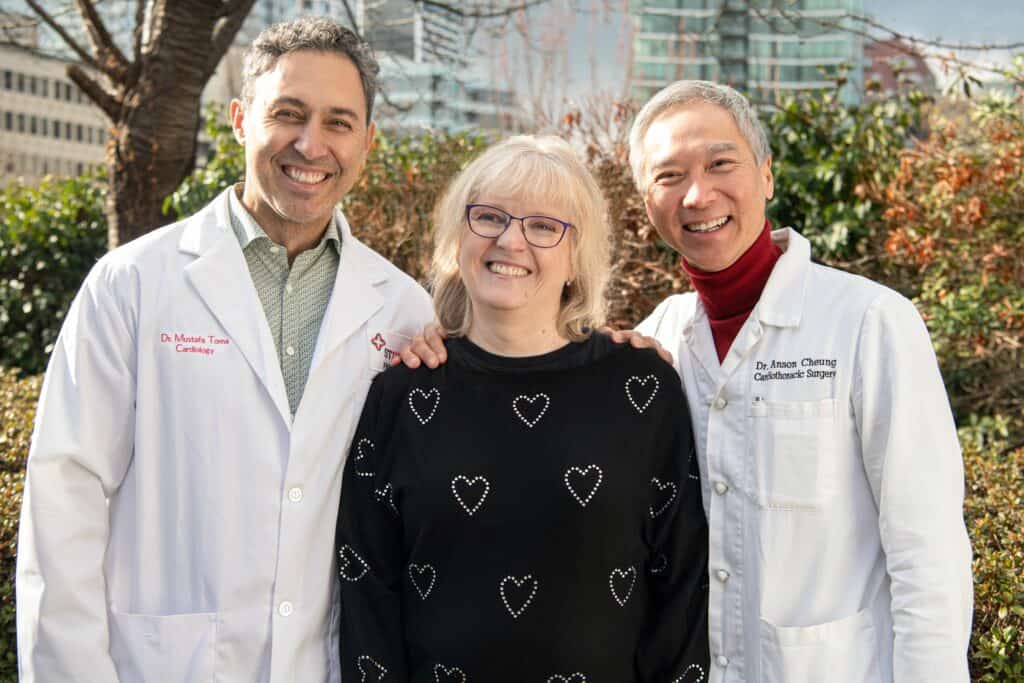
“We ended up doing quite a unique set-up for her to give her the most optimally functioning defibrillator,” explains Dr. Jamil Bashir, a cardiac surgeon at St. Paul’s Hospital and the head of Vancouver Coastal Cardiac Surgery and the UBC Division of Cardiac Surgery.
This treatment, designed specifically to suit her lifestyle and needs, became emblematic of the compassionate care Roberts would continue to receive at St. Paul’s.
“Dr. Bashir was amazing. I think of him every morning when I see the scar and am so grateful,” says Roberts.
What is even more unique about this situation is Roberts and her partner didn’t have any family here in Vancouver. And so, the staff at St. Paul’s stepped in and became her support system – particularly the nurses, who she became quite close with during her time in hospital.
“It made my day seeing a familiar, friendly face and feeling reassured that I was in good hands when I was vulnerable,” she says. “I couldn’t have visitors. At one point I was missing chocolate, so the nurses would bring me in little pieces of chocolate. The smallest touches of genuine compassion meant the world to me.”
Another St. Paul’s health care provider who made an impact on her care was Dr. Scott Apperley, a respirologist. Since Roberts’ diagnosis in 2020, Dr. Apperley has helped manage her GPA, which can cause airways to narrow and some of the lobes of the lungs to collapse.
A game changer for Roberts was an Erbecryo machine, which was purchased thanks to St. Paul’s Foundation donors. The machine allows specialists to freeze and remove extra tissue in her lungs to reduce inflammation.
Beginning in 2021 until June 2023, the medical team performed bronchoscopy procedures – where a thin, lighted tube is used to look directly at the airways in the lungs – on Roberts. Since June 2023, the team has used the Erbecryo machine leading to longer and longer intervals between treatments.
“With use of that over time, it has really improved the airway calibre and hopefully has resulted in a greater longevity of keeping those airways open,” Dr. Apperley says. His hope is that Roberts will reach a stage where these treatments aren’t needed at all.
“Every single person has gone above and beyond. And it’s not just that they literally saved my life. The care team has allowed me to reclaim my life and do things that I never thought possible. Now I’m really encouraged about what I can do next.”
Karam Roberts
Since her release from hospital, Roberts has ferociously pursued her own recovery, visiting the gym, participating in St. Paul’s Healthy Heart (a community program for people with or at risk of developing heart disease), and running the BMO Vancouver Marathon eight kilometre race last May. She was even inspired to hike the Beehive trail in Lake Louise – a 20-kilometre round-trip hike with an elevation gain of 1,140 metres.
When she reached the top, Roberts says the profundity of her journey really hit her. “I never, ever thought I’d be able to do this.” She was finally living the dream that brought her to Canada.
Making miracles routine
The care and collaboration exemplified in Roberts’ case will be streamlined at the new St. Paul’s Hospital. The 1.2-million-square foot acute care hospital will be connected to the new St. Paul’s Clinical Support and Research Centre (CSRC), an innovation hub that will accelerate personalized and effective treatments that enhance quality of care and overall well-being.
The hospital’s new infrastructure will streamline the patient journey, ensuring patient care areas are close to the critical care services they require. Dr. Bashir is also hopeful that the CSRC will empower medical staff to offer new types of procedures – such as those that have given Roberts a new lease on life.
“I have a lot of aspirations for new ways to care for patients and to continue to do what we’ve done over the last 130 years, which is to do our best to care for people in a compassionate way,” says Dr. Bashir.
And this kind of care brought Roberts back to life.
“It’s not just one individual. It’s everyone together,” she says. “Without them, I wouldn’t be where I am today.”
Support the future of collaborative, compassionate health care by donating to the nSPH and the CSRC.