Published Promise 2023
Sophia Draper was born with a complex heart condition and had the first of her many surgeries while still a baby. She spent her first 18 years under the care of specialists at BC Children’s Hospital, establishing relationships with doctors and nurses at the hospital, as well as friendships through the BC Children’s Heart Network with kids who shared similar medical experiences. The cocoon came to feel like family.
Then she turned 19. And even though her condition would require lifelong treatment, she aged out of the only care she had ever known.
“I had to leave Children’s behind and transfer to the congenital heart clinic at St. Paul’s,” Draper remembers. “At my last appointment at Children’s, everyone gathered to say their goodbyes.” It was an overwhelming experience.
A lifeline for hundreds of youth each year
This is a truly significant time in the lives of these young people. Not only are they are testing the waters of adulthood with jobs, college, and relationships, they’re also transitioning from the protective world of pediatric care into the adult system.
For many, it can be so intimidating that even something as minor as parking or transit fares can be barriers to care. And with young patients coming to St. Paul’s from across BC, travel can become another roadblock. If it starts to feel overwhelming, there’s a serious risk they’ll skip their appointments, neglect their medications, or pretend their condition is less serious than it is.
But the reality is, the choices these young adults make during this crucial time will define their health and wellness for the rest of their lives.
This is a time in life when they’re developing socially and experiencing transitions related to school and entering adult life as well. Combined with dealing with a chronic illness, it definitely makes it a more vulnerable time for these young patients.
– Vanessa Lewis
Enter the Scotiabank Youth Transition Program (SYTP). Founded in 2019, the SYTP provides a safety net – unique in Western Canada – to help newly-minted adults with complex medical conditions begin managing their own health care.
For young people accustomed to the colourful child-centred approach of pediatrics, the adult world can seem cold and even unfeeling.
“Young people transitioning to the adult program can find it an extremely isolating and daunting process; however, both the pediatric and adult care services recognize the importance of making this process seamless and are invested in helping grow the transition program,” says Dr. Gnalini Sathananthan, a congenital heart specialist with the Yasmin & Amir Virani Provincial Adult Congenital Heart Program (VPACH) at St. Paul’s Hospital.

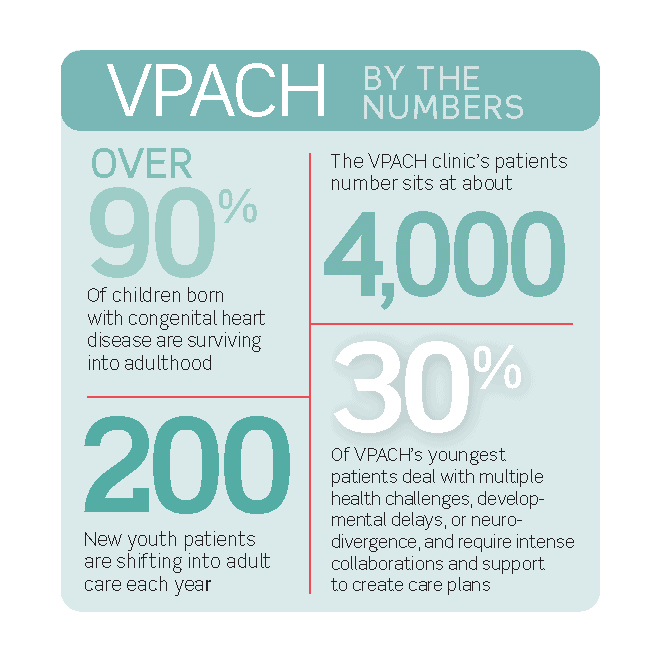
Sixty years ago, fewer than 20% of babies born with congenital heart defects reached adulthood. Today, it’s more than 90%. Each year, VPACH adds about 200 new youth patients to its 4,000-patient roster.
The sheer number of patients and their complex needs present the team with some unique challenges.
“Approximately 30% of patients seen in the VPACH clinic have intellectual and developmental disabilities,” says Dr. Sathananthan. “Their care requires intense collaboration and multidisciplinary support.”
It’s not just those with congenital heart disease needing meticulous, personalized care. The same is true for youth with any serious chronic health concern. Thankfully, the SYTP helps empower young adult patients to truly feel like they’re supported by their caregivers, in control of their health, and invested in their own care.
Building confidence with compassion
Emma Iacoe, leader of Program Development for the SYTP, with the help of stakeholders, developed five pillars the team uses as their north star. To wit: youths need to feel welcome; they need access to supportive services that address their physical and emotional well-being; they need to be monitored regularly to gauge how they’re feeling and ensure they’re following their care plan; and they need to create strong connections with peers going through similar experiences.
Eager to bring this wrap-around care to young people with heart disease across BC, the SYTP is piloting programs in VPACH and the Hemoglobinopathy program at St. Paul’s.
Once the pilots are complete, the hope is to expand to other programs and clinics at Providence Health Care that have youth transitioning. The team is also hoping it will lead to workshops, a youth-friendly website, handbooks, videos, and social media tools to create an even more robust program.
Dr. Sathananthan stresses that a successful transition into adult care must embrace and start the process early, several years before these adolescents actually transition to adult care. “We’ve done so much to advance the medicine in congenital heart. The next big step to wellness is providing psychosocial and educational guidance so that these young adults can support themselves through their adult lives.”
Setting up for success with the Scotiabank Youth Transition Program
What does a successful transition from pediatric to adult care look like?
The SYTP leaders have developed a framework to set up their new patients for success from the get-go. Of course, patients’ conditions are monitored and treated, but they are also provided with a network of resources to learn about self-management until they’re ready to take on the mantle of their ongoing care.
Draper, who’s now a graduate student in speech and language pathology at McGill University, recalls her early days at St. Paul’s as a time of growth. “I had to learn a lot in a short time! I’m glad I didn’t have to do it alone.”
To donate and help the VPACH team expand their provincial reach and improve access to care, visit donate.helpstpauls.com/SYTP.