Published Promise 2024
Diagnosed with cystic fibrosis (CF) at 16 months, Kim Wood never truly knew what it felt like to take a full breath.
Thanks to the dedicated health care staff and her parents’ careful commitment to a supportive health regime, Wood fared quite well during childhood and young adulthood with a degenerative, chronic disease. In fact, she was so inspired by the caring treatment she’d received all her life she became a pediatric nurse.
When Wood reached her early 20s, her health took a downward turn. As her illness progressed, Wood experienced frequent lung infections that required hospitalization. Thick, sticky mucus pooled in her lungs, making it difficult to breathe. As her lung function declined and she spent more time in the hospital than out of it, Wood made the difficult decision to take an extended leave of absence from the career she loved to focus on her wellbeing.
Her body no longer felt like her own – her life revolved around tracking her medications, protecting her immune system from infection, sleeping, adjusting plans, wondering if treatments would remain effective, and endless anxiety about what would come next. Wood eventually adapted to the unpredictability with grace.
“There were many times that I had to miss out on family reunions, destination weddings, or vacations because I had an exacerbation,” she says. “I learned that it was a lot easier to keep your expectations low and just roll with it.”
Still, life went on – Wood fell in love, got married, and began to plan for a family. Shortly after the birth of her son (via a surrogate), Wood’s deteriorated to the point where was referred for evaluation at BC’s lung transplant clinic.
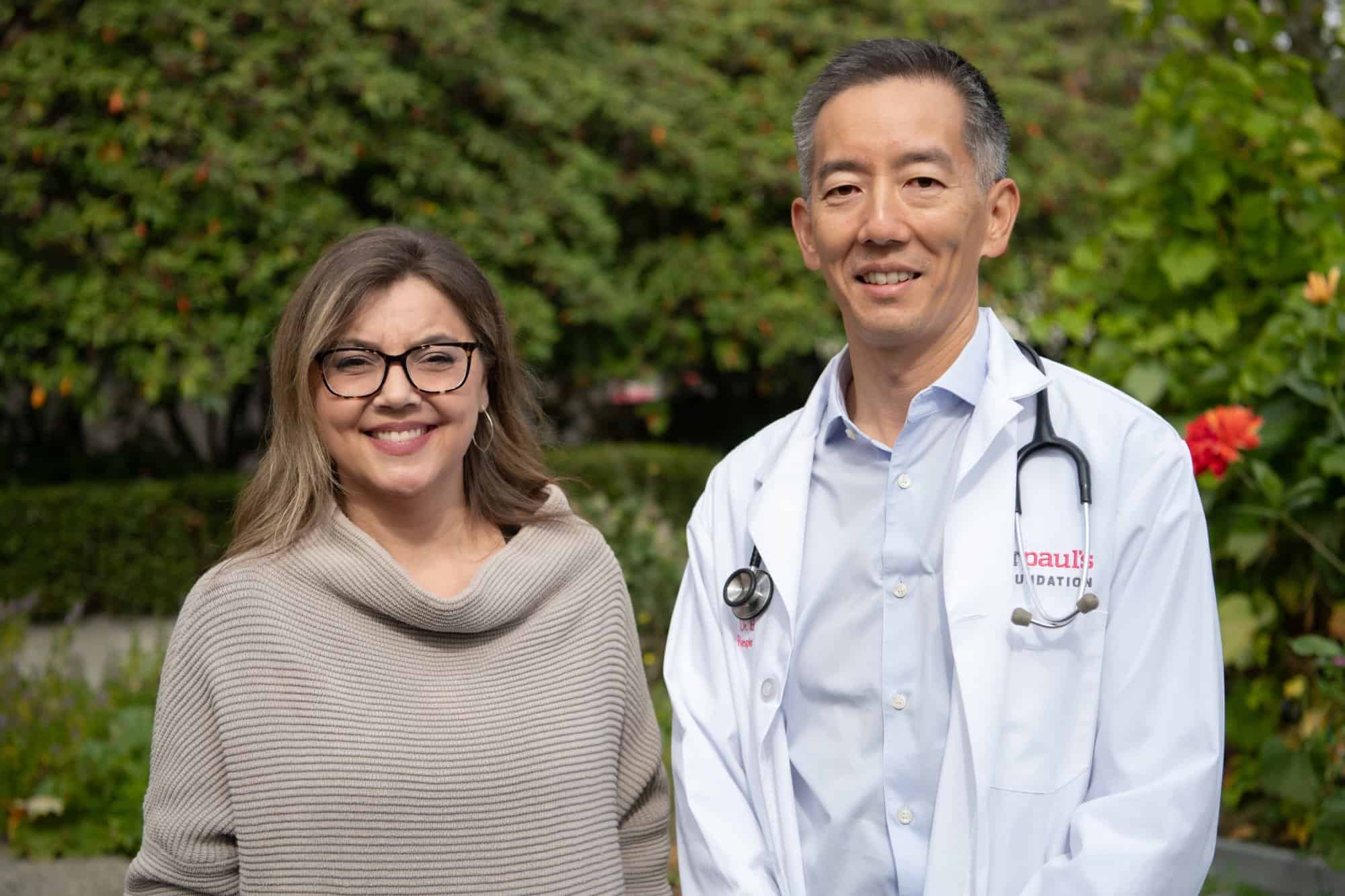
Then came Dr. Bradley Quon and his clinical trial evaluating Trikafta at St. Paul’s Hospital.
Helping patients with cystic fibrosis breathe again
Cystic fibrosis is a genetic, progressive, and fatal disease. It primarily affects the lungs and digestive system. The lungs don’t clear secretions properly, and mucus accumulates – causing infections and scarring. It can be so difficult to breathe that a patient can feel like they’re drowning. Eventually, the lungs become so damaged they don’t work anymore, requiring transplantation – that is, if a new set is available.
Not that long ago, CF was a death sentence: most patients didn’t live to adulthood. In 1979, St. Paul’s Hospital opened one of the first stand alone adult CF clinics in North America, and has continued to advocate for new treatments and trailblazing care. While there still isn’t a cure, thanks to modern therapies patients are now living full, long lives.
And doctors like Dr. Bradley Quon are paving the way for better, life-changing treatments – and an eventual cure.
Dr. Quon is a clinician-scientist at St. Paul’s Hospital. He’s the medical director of the CF Adult Care Program, and a researcher at the Centre for Heart Lung Innovation. In 2018, because of its global reputation, St. Paul’s became one of only five clinical trial sites in Canada for a new drug called Trikafta.
At this point, the drug was in phase three of development, which is the last phase before approval from Health Canada. During a Phase 3 trial, researchers are looking to see if a new treatment performs better than the standard one.
For Wood, the birth of her son bolstered her desire to find a solution to her declining health. As a patient of Dr. Quon’s, she expressed interest in participating in the Trikafta trial.
“When I first met her, I was just struck by her tenacity, her strength, and her willingness to do everything possible to keep her lungs healthy,” says Dr. Quon.
“Oh my gosh, this is what breathing is supposed to feel like”
Wood’s health status meant she was a prime candidate for the Trikafta trial. Since the study was double-blind, she didn’t know if she would receive the placebo or the real medication.
Within 24 hours of her first dose, Wood felt certain she was taking Trikafta due to the intense change in her lungs. After a couple of weeks, she was amazed to discover she was breathing in a way she’d never experienced.
“I started to feel that complete, unrestricted breath. It was astonishing because I had never felt this, even when I was really young on a good, healthy day,” Wood recalls. “I was like, ‘Oh my gosh, this is what breathing is supposed to feel like’. It was absolutely mind-blowing.”
And it wasn’t just Wood’s breathing that improved – she suddenly felt full of energy and could function on less sleep (a critical asset when raising a newborn!).
As Wood’s treatment continued, she also noticed she experienced fewer colds and cases of the flu; and if she did catch a cold, it didn’t land her in the hospital. Like many of us, she could simply heal and get on with her life.
Letting go of the back-up plans, and being the mom she always dreamed of being

Wood’s experience is a mirror of what many other patients felt taking Trikafta, too. The drug trial showed a dramatic improvement in patients’ lung function and quality of life, as well as reduced hospitalizations. In 2022, the drug was approved by Health Canada and has continued to enhance the lives of patients like Wood.
“It’s truly a miracle breakthrough,” Dr. Quon says. “Seeing such a dramatic response right away is what any researcher would hope for, and that’s the impact that research can have on our patient care. We’ve seen Trikafta fully change lives.”
And Wood counts herself as a person whose life has changed for the better because of Trikafta and all the innovative research occurring at St. Paul’s.
“My life would have been so different had I not started on Trikafta,” she says. “My child’s life would have been very, very different. I never thought I was going to be able to be the kind of mom that I wanted to be.”
Wood and her husband spent a significant amount of time discussing the realities of cystic fibrosis as they planned for their family – including the possibility that her husband might become a single dad. Wood feared she’d only be able to parent from the couch or spend precious moments with her child from a hospital bed via video chat.
Now that Wood has a successful drug treatment, her family has begun to let go of their contingency plans. She can fully engage with her young son – attending school events and concerts, volunteering for field trips, playing with him, travelling – and all without constantly worrying she’ll get sick.
“My cystic fibrosis is definitely not at the forefront anymore. There was a time where I would get so resentful towards CF because all of my memories felt like they were dictated by it,” she says. “Now we can make plans. My son’s looking forward to going to Legoland [and to] Disneyland, doing family vacations, and really making memories. It’s so different. The change is just indescribable.”
The work isn’t quite done yet – and you can help
Trikafta is a transformational drug, but it’s only approved for people with certain types of cystic fibrosis. It’s been shown to be effective for 85-90% of patients with the most common CF mutations. While Trikafta has the potential to work for the remaining 10-15%, patients with rarer mutations weren’t included in the original trial.
That means Trikafta – a $300,000 annual treatment – isn’t covered for that smaller group of patients who want to try it.
“We’re trying to close that gap and make sure that no one is left behind,” says Dr. Quon.
Dr. Quon’s next stage of research takes nasal cells from patients and grows them in the lab. Then, he applies Trikafta to see how those cells respond to treatment. This is an example of precision medicine, where the doctor can uniquely tailor the medication to the patient.
But Trikafta won’t help all patients. Out of the 10-15% of people with rare mutations not eligible for Trikafta, Dr. Quon anticipates only half will respond to the drug. For the remaining half, we’ll need other innovative solutions. Upcoming clinical trials will involve genetic-based therapies that correct or replace the defective gene.
And the new St. Paul’s Hospital and medical campus will be a prime destination to perform these trials. The Clinical Support and Research Centre – connected to the acute hospital – will feature a larger space, state-of-the-art equipment, improved facilities, and the ability to conduct more clinical trials, enabling clinicians like Dr. Quon to amplify their research and help more people like Wood.
“We are at the forefront of both research and clinical care. Working adjacent to the hospital, we can easily take discoveries in the lab and translate them into better treatments for our patients. Ultimately, we want to make CF stand for ‘cure found’. At that point, I may be out of a job, but I’m so grateful for the impact that would have on our patients.”
Dr. Bradley Quon
Wood is eager for more patients with CF to discover what it’s like to breathe again.
“Every day I wake up, look at my Trikafta package and I feel grateful for having the privilege to take that medication and have it affect my body in the positive way that it has,” she says. “I don’t know if I would be here without Trikafta, and I don’t know if I would be able to be the kind of mom I’ve always wanted to be for my little boy.”
We need your support to continue to pioneer health care transformation in BC.