Leaders in life-changing, patient-centred medical research
Good research helps us better understand patients and residents, and what they need to thrive.
Our research is grounded in compassion, and patients inspire us to innovate every single day. Their real-world challenges drive and inform our research – pushing us to create better solutions and life-saving medical breakthroughs, which are then taken from the lab bench to a patient’s bedside as soon as possible.
At its core, St. Paul’s Hospital is a purpose-built research facility that attracts the best and brightest clinician scientists because we’re never satisfied with the status quo. When a patient comes through our doors, our focus is on using the most up-to-date medical research to advance their care and help them live their optimal, most meaningful lives.
We’re on the cusp of a new age in research with the promise of not only treating life-threatening conditions, but discovering how to prevent them in the first place.
Made in BC innovations that are changing the world
PHC has a remarkable 130-year legacy of compassion, social justice, and driving innovation.
Our researchers witnessed what patients needed, and then created solutions to help. Many of these groundbreaking innovations, which began with a single person or a small population in need, have since changed the world.
Our Innovations
-
Dr. John Webb pioneered a minimally invasive way to replace heart valves without open heart surgery. TAVI is now the gold standard in more than 40 countries and has helped 450,000 people. Even Mick Jagger has had the procedure!
-
St. Paul’s was the first hospital in BC to provide care to AIDS patients when the epidemic emerged in the 1980s. It was here that Dr. Julio Montaner developed HAART (highly active anti-retroviral therapy). His treatment protocols have transformed HIV from a death sentence to a chronic, manageable disease – saving millions of lives around the world.
-
When Dr. Steve Mathias recognized the urgent need for youth-specific mental health outreach, his idea became Foundry: a place where young people can drop in and get support for mental wellness, substance use, family dynamics, employment, and social connection all under a single roof. Today, there are 16 Foundry centres currently open, 9 in development, and 10 additional funded but not in development. The aim is to have 35 centres open by 2027.
-
Dr. Marc Deyell is leading the first-in-BC trials of a revolutionary new device to treat patients with atrial fibrillation. This frightening heart condition affects more than 200,000 Canadians and can increase your risk of stroke by 500%.
-
Dr. Jim Russell is the top ranked doctor in the world for septic shock research. Dr. Keith Walley has been appointed a member of the Order of Canada for his innovative research in the field of sepsis and septic shock. Work by Dr. Russell, Dr. Walley, and their colleagues at the sepsis lab at St. Paul’s led to a game-changing sepsis drug treatment shared around the world.
-
Dr. Fariba Mohtashami developed a safer, less invasive way to remove uterine fibroids. Using a minimally invasive laparoscopic technique (sometimes called keyhole surgery), the majority of large fibroid tumours can be excised without removing the entire uterus.
-
Dr. Mari DeMarco pioneered a first-in-Canada Alzheimer’s biomarker testing program, which helps identify the early stages of the disease so patients can access treatments earlier that improve their quality of life.
-
Respirologists Dr. Chris Ryerson and Dr. Alyson Wong established our first Post-COVID Respiratory Clinic and research program, which later expanded to our Post-COVID Recovery Clinic to address the full scope of the illness. Their research, in collaboration with hospitals across the country, was the first to show a correlation between auto-antibodies (proteins that can cause harmful reactions in our bodies) and long COVID.
-
The lab at St. Paul’s became the first in Canada with fast, fully automated COVID-19 testing. And when chemical supplies needed to process samples ran low, Dr. Daniel Holmes and his teams figured out a clever workaround to batch-test results. During the COVID pandemic, we had the highest testing capacity of any lab in BC, and we were the only hospital lab in Canada doing whole genome sequencing of the COVID-19 virus.
-
COVID isn’t the only public health emergency this province is facing. With fatal drug poisonings on the rise, Dr. Brittany Barker launched a study to learn more about vaccination rates in urban populations, including those who use unregulated drugs. The study’s findings offer guidance to health care professionals about how to resolve barriers to, and mistrust of, health care.
-
Six British Columbians die from an overdose every single day. Road to Recovery, a first-of-its-kind, evidence-based initiative, is transforming substance use treatment by providing a seamless continuum of care services all in one location. These investments will create 25 acute stabilization and withdrawal management beds, and 20 transitional stay beds at the current St. Paul’s Hospital, all of which will be relocated to the hospital’s new campus when it opens in 2027. An additional 50 PHC recovery beds will be created in the community in close proximity.
-
For the first time in history, there are more Canadians over the age of 65 than under 15. That’s why PHC and Providence Living are pioneering a whole new model of care for older adults in acute care and for residents in long-term care. We’re developing a brick-and-mortar Centre for Healthy Aging on the campus of the new St. Paul’s Hospital. And we’re building Canada’s first public, non-profit care village (based on the dementia village concept).
A strong reputation in medical research excellence
Right now, teams of scientists at PHC are in pursuit of some of the world’s most promising research. Among their initiatives:
Learn more about the myriad of ways we’re currently using AI in health care.

The ultrasound of the future
More than 600,000 British Columbians live in rural communities and small towns – and they need the same quality of care as their big-city counterparts. Just 5% of BC physicians are trained to analyze scans, and up to 40% of patients face lengthy wait times for the tests. What if the vital, life-saving help you need is hundreds of kilometres away?
Enter PoCUS, a breakthrough imaging technology (the name stands for Point of Care Ultrasound). It’s a small, wireless “scanner” that takes ultrasound pictures and video inside almost any part of the body and displays them on any mobile phone or tablet.
With PoCUS, patients have access to ultrasound scans no matter where they live. PoCUS equips doctors with wireless handheld ultrasound devices, e-learning, and visual feedback in real time. A family doctor can scan a patient, talk to a world-class doctor at St. Paul’s, and then deliver faster, more accurate diagnoses.
This game-changing technology is being used to diagnose critical heart problems, COVID-related lung issues, and more.
“The project will allow primary care providers to acquire clinically relevant data at the patient’s bedside,” says Dr. Oron Frenkel, an emergency physician at St. Paul’s. “Some scans produce results that are clinically significant in seconds. Of course, the ultimate winners are the patients who can get faster diagnoses.”
Making quicker COVID diagnoses
It can be challenging to tell the difference between COVID and other respiratory conditions.
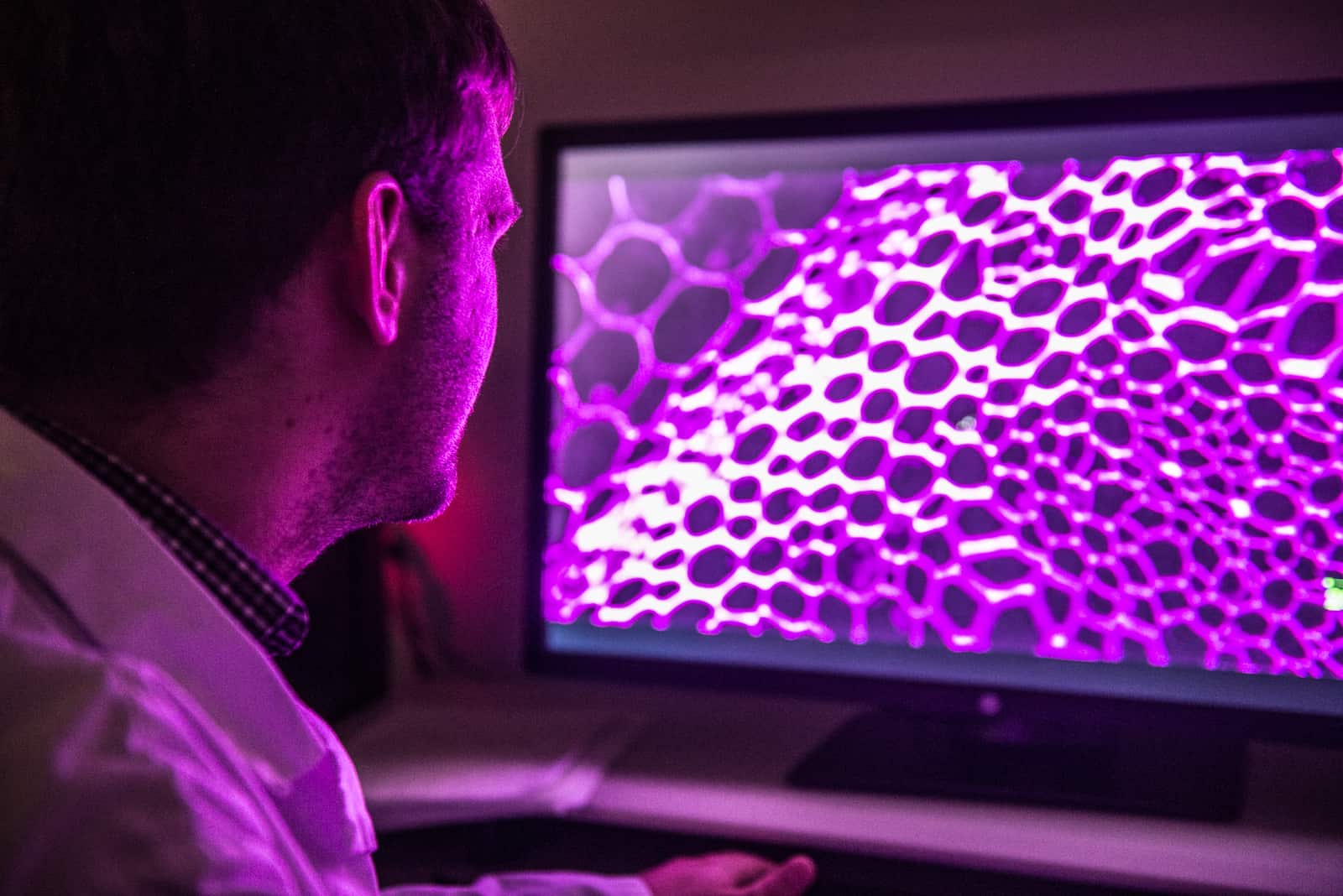
A new AI device, developed in partnership with Simon Fraser University, is helping busy doctors and frontline health care workers accurately diagnose COVID-19 quickly, so they can provide the best patient care.
The tool enables a clinician to feed a patient’s chest X-ray image into a computer, run a bio-image detection analysis, and determine a positive pneumonia case that is consistent with COVID-19.
This AI system can also help less experienced doctors look over a data set and make a quick diagnosis before a senior doctor can step in.

Accessing the most comprehensive patient data
Information is power: and the more information, the better.
And when researchers have access to 2.7 million medical images from over 300,000 unique patients, they’re better equipped to unlock new discoveries and improve patient care.
The Integrated Health Informatics Datalab (IHID) is a made-at-PHC platform, in partnership with PHC Ventures. It collects, analyzes, links, and shares de-identified health data from many sources, providing high quality data sets in a secure environment.
This saves an immense amount of time, giving researchers the ability to focus on new discoveries that address unmet clinical health care needs.
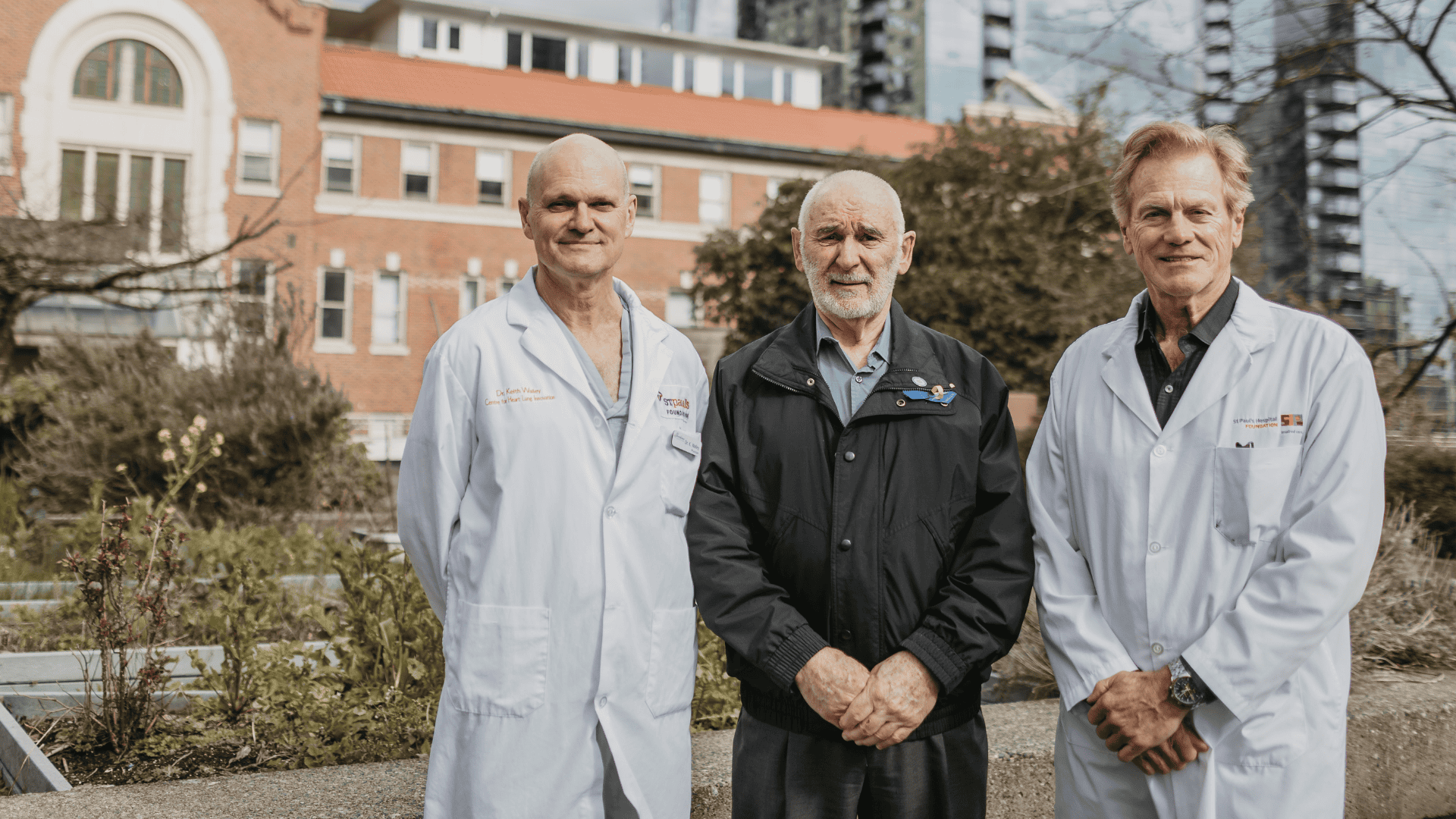
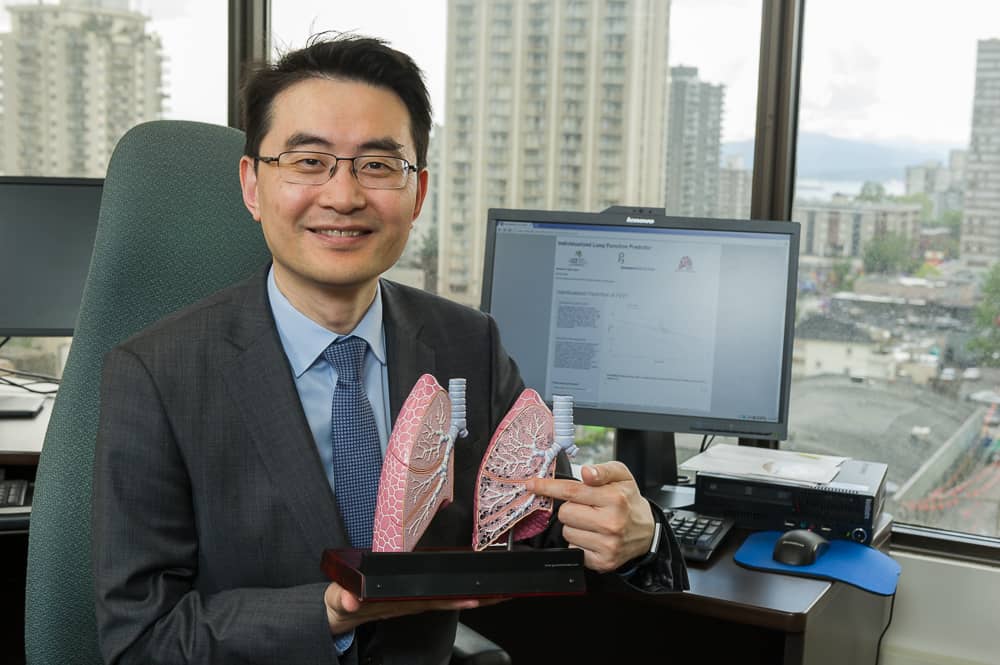
Preventing the number one cause of death worldwide
James Stitchman was admitted to St. Paul’s with a life-threatening sepsis infection at the height of COVID in 2021. Fortunately, St. Paul’s has the top-ranked doctor in the world for septic shock research, Dr. Jim Russell. Within nine days, James recovered and returned home to his family.
Sepsis is the leading cause of death worldwide, causing 11 million fatalities each year – that’s more than heart attacks or cancer. Research by Dr. Russell and the sepsis lab at St. Paul’s led to a game-changing sepsis drug treatment shared around the world – and now they’re using artificial intelligence to predict sepsis risk.
Dr. Russell is developing an AI model that will take patients’ vital signs and, combined with their unique genetics, predict if they are at risk of developing sepsis – allowing doctors to catch and treat sepsis much earlier.

Comprehensive hospital care from the comfort of your own home
Patients who have been hospitalized for significant health issues often remain in the system for basic supervision and monitoring while they heal. What if they could do their healing safely at home?
The Hospital at Home program is a new digital platform improving the quality of at-home care for discharged patients. It uses AI and home monitoring technology to take care of patients at home, saving hospital resources for acute cases.

Meet Tarzan and Jane, St. Paul’s newest lab techs
The busy laboratory at St. Paul’s processes over 145,000 microbiological samples each year from BC and the Yukon.
Now, for the first time in Western Canada, a set of robot lab technologists – named Tarzan and Jane – are handling up to 70% of those samples!
This sophisticated technology, called Walk Away Specimen Processing Lab (WASPlab), is an efficient and scalable way to transfer patient specimens onto culture plates – making it easier and quicker for staff to analyze and ultimately, treat patients sooner.
“In order to optimize patient care, we want technologists to concentrate on the more complicated analytical laboratory work, the more interpretive work that requires human thought,” says Dr. Marc Romney, head of Medical Microbiology and Virology at St. Paul’s. “We don’t want technologists to be performing manual work that machines and robots can easily take on.”
The future of health care at the csrc
-
The Innovation Centre will be a dynamic, collaboration hub with a variety of meeting spaces and sandboxing prototyping areas that enable partnership and commercial enterprise in life sciences.
The floor is designed to be a symbiotic and social ecosystem that brings people out of their labs and offices into a space that inspires them to share their ideas, creativity, problem-solving, projects and discovery. It will stimulate knowledge transfer and exchange in a ‘collision space’ where ideas can come to life.
-
The new St. Paul’s is being deliberately designed as the most data-driven and digitally fluent in Canada. The purpose-built data centre will maximize data for improving health outcomes, and also generate partnerships.
The CSRC and its Innovation Centre will also be a vibrant training ground for research and evaluation, and preparing a new generation of innovators, intrapreneurs, and entrepreneurs who will define our future.
-
Our multidisciplinary laboratory building will centralize the management of resources to discrete cores. This will optimize the shared use of specialized equipment and instruments to support the increased need for flexibility, efficiency, and collaboration among teams.
-
We’ll be one of the only facilities in Western Canada with the potential to conduct all three phases of non-cancer clinical trials. This will enable our scientists to develop critical, life-saving treatments and take them from concept to completion, bring them to patients quicker, and keep our patented therapies within BC.
-
Attached to the potential clinical trials unit, there is an aspiration for a simulation centre where researchers, staff, students, and industry can explore ideas and exchange knowledge. The prospect of practicing the latest techniques through realistic digital simulations has the promise of expanding clinical trial capacity to improve accuracy and produce the best results for patients
Your support helps deliver visionary treatments to patients and their families. We are ready to bring more life-saving discoveries to BC, across Canada, and around the world. Learn how you can be part of the future of medicine at St. Paul’s.