Published Promise 2023
Two years ago, James Stitchman was spending much of his retirement writing a book with his young grandson and enjoying brisk walks along Vancouver’s seawall. Then he got COVID-19, and everything changed. One morning, his wife found him unable to communicate or understand what she was saying. She took him to St. Paul’s Hospital. He spent nine days there, struggling to breathe and in a state of confusion.
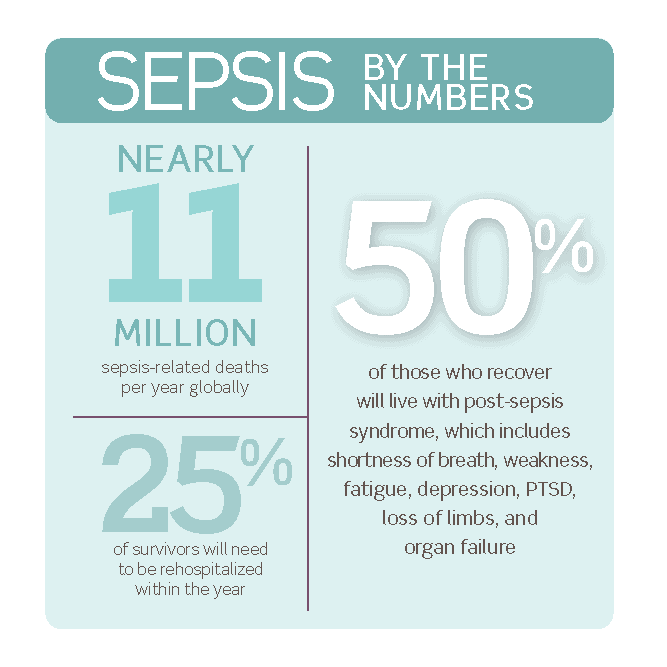
Stitchman had developed sepsis, an aggressive infection triggered, in his case, by COVID-19. The syndrome can cause rapid, widespread organ failure affecting the lungs, kidneys, brain, and heart.
Sepsis is the number one cause of death worldwide, but early recognition and treatment can reduce mortality by half. For Stitchman, the quick recognition and care he received at St. Paul’s saved his life.
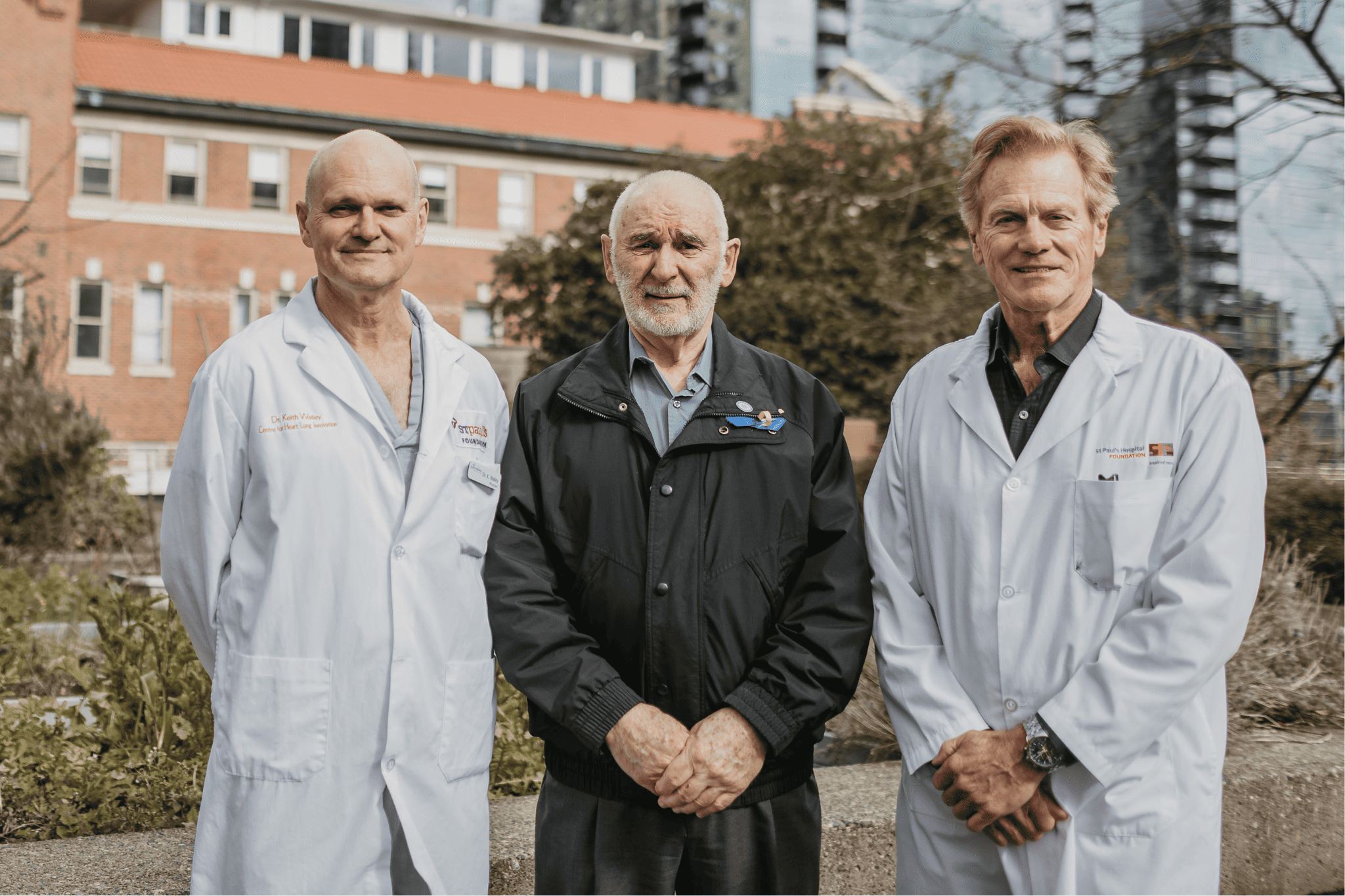
“I was one of the lucky ones. I got to go home again,” says Stitchman, who subsequently experienced memory problems and shortness of breath for about a year. “I don’t have any recollection of some of my time at St. Paul’s. I was a lost soul for a few days there. But I had a great team pulling for me. I appreciate everything St. Paul’s did for me.”
Sepsis is getting increased attention due to its association with COVID-19. That’s because we’ve learned that COVID itself isn’t the killer. Rather, COVID is a viral infection, often involving the lungs (called pneumonia), that triggers an out-of-control immune response, which is sepsis. And it’s the sepsis that causes organ failure leading to death.
And the reason sepsis is so challenging to treat? There’s no specific, proven medication for it. It’s a complex syndrome that can require antibiotics, oxygen, drugs to stabilize blood pressure, and dialysis to support failing kidneys. In addition to this, there’s also no diagnostic test available to detect sepsis, making the diagnosis a challenge.
Globally renowned septic shock research

Long before the pandemic, the team at the Centre for Heart Lung Innovation (HLI) at St. Paul’s was developing the first new treatments for sepsis since the introduction of antibiotics in 1941. Today, HLI is the leading sepsis laboratory in the world, with the most breakthroughs and the most impactful research.
“Few people know that more people die of sepsis than of heart attack. About one in three who get sepsis will die within one month. It is worse than cancer, worse than heart attack, and worse than heart failure.”
– Dr. Jim Russell
“The pandemic we’ve all been living through is actually a pandemic of sepsis due to COVID-related pneumonia. Everybody who dies of COVID actually dies of sepsis and pneumonia. Everybody,” says Dr. Russell.
As the top ranked doctor in the world for septic shock research, Dr. Russell knows how prevalent and devastating sepsis can be. And that is exactly why, together with his colleague, Dr. Keith Walley – another global leader in septic shock research – they are focusing on discovering and understanding the mechanisms behind sepsis.
The duo has co-published scores of studies in esteemed medical journals including the New England Journal of Medicine. And, they’ve seen more than 10,000 ICU patients with sepsis over their careers.
“We have a really wonderful collaboration because Dr. Russell’s clinical trials often arise from ideas in the lab,” Dr. Walley says. “Over the last 35 years, what we’ve accomplished has changed global sepsis practices and improved survival rates.”
High tech hope
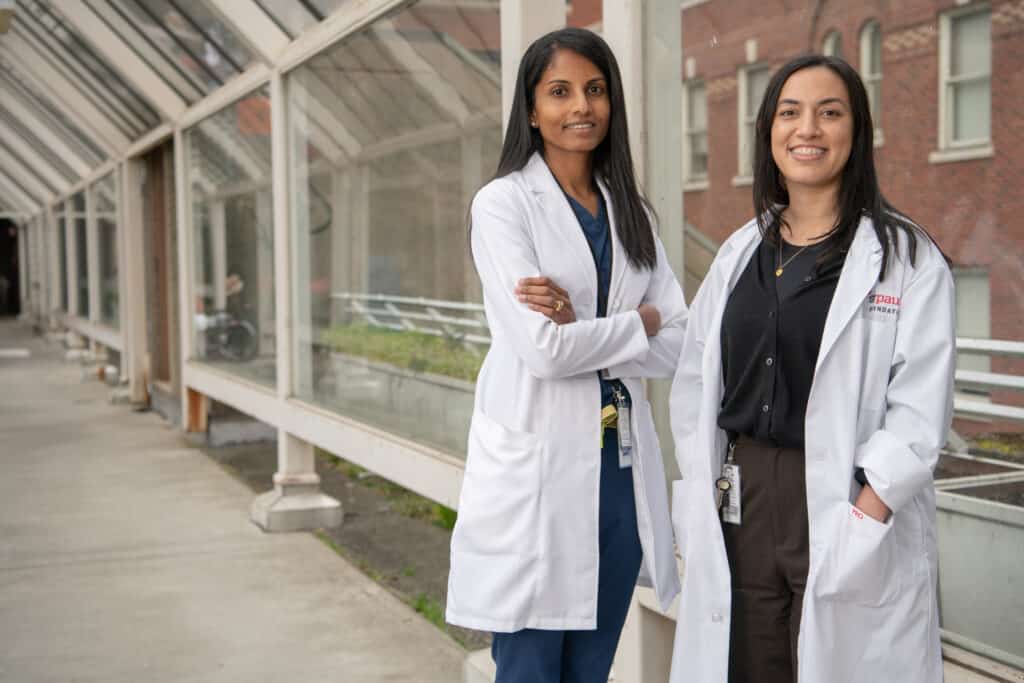
Drs. Russell and Walley are leading new research that could be a game-changer in sepsis treatment, examining how a class of drugs called PCSK9 inhibitors, currently used for heart disease and stroke, could treat sepsis.
“We were the first in the world to discover that people with a defect in their PCSK9 gene have a better survival rate,” Dr. Russell says. “And our discovery led to others doing a recent trial of a PCSK9 inhibitor showing significantly decreased mortality of acute COVID-19.”
To go even further with their promising research, the pair have their sights set on the creation of a Chair in Critical Care. This senior academic research role will focus on critical care medicine and sepsis, which go hand-in-hand. As a first-in-Canada initiative, the new Chair will take HLI’s work to the next level with research that could yield drug discoveries, new treatments, and better outcomes for British Columbians and people across the globe.
As for Stitchman, he recovered from his sepsis ordeal and is now back to strolling the seawall. And he even finished the book he was writing with his grandson. (It’s called Thunder and the Werewolves.)
“James’ story inspires me to do this research,” says Dr. Russell. “It could have been a tragedy for this family. Now he’s back to living his life. If we continue to recruit brilliant scientists, we can keep St. Paul’s at the forefront of science and research. And we can make everyone’s experience with sepsis more hopeful.”
Make an impact at a global level with health care by helping us fund a Chair in Critical Care. Give today at donate.helpstpauls.com/Sepsis.