Where science meets compassion
St. Paul’s Hospital sits on the frontline of the toxic drug crisis.
Each year, we treat thousands of patients for problematic substance use. This is rarely a person’s only health concern. Fully 70% of the mental health patients treated at St. Paul’s Hospital also have a substance use disorder. And in just the last five years, visits related to mental health and substance use have increased by 76%.
For people in crisis, accessing the right care when they need it can be extremely challenging. So we meet our patients where they are – at St. Paul’s and in the community. We ensure they feel welcomed with culturally-appropriate, trauma-informed care. And we support them in their journey of recovery.
For many patients, the first stop is St. Paul’s Teck Emergency Centre. Because one size does not fit all for anyone in the emergency department, we triage and treat substance use patients with a variety of specialized programs and services.
- Mental Health, Urban Health, and Substance Use teams for specialized inpatient care and outreach in the community.
- Rapid Access Addiction Center (RAAC) for low-barrier outpatient services.
- The HUB for care in a private setting outside the ED.
- Transitional Care Centre for a bridge between care at St. Paul’s and care in the community.
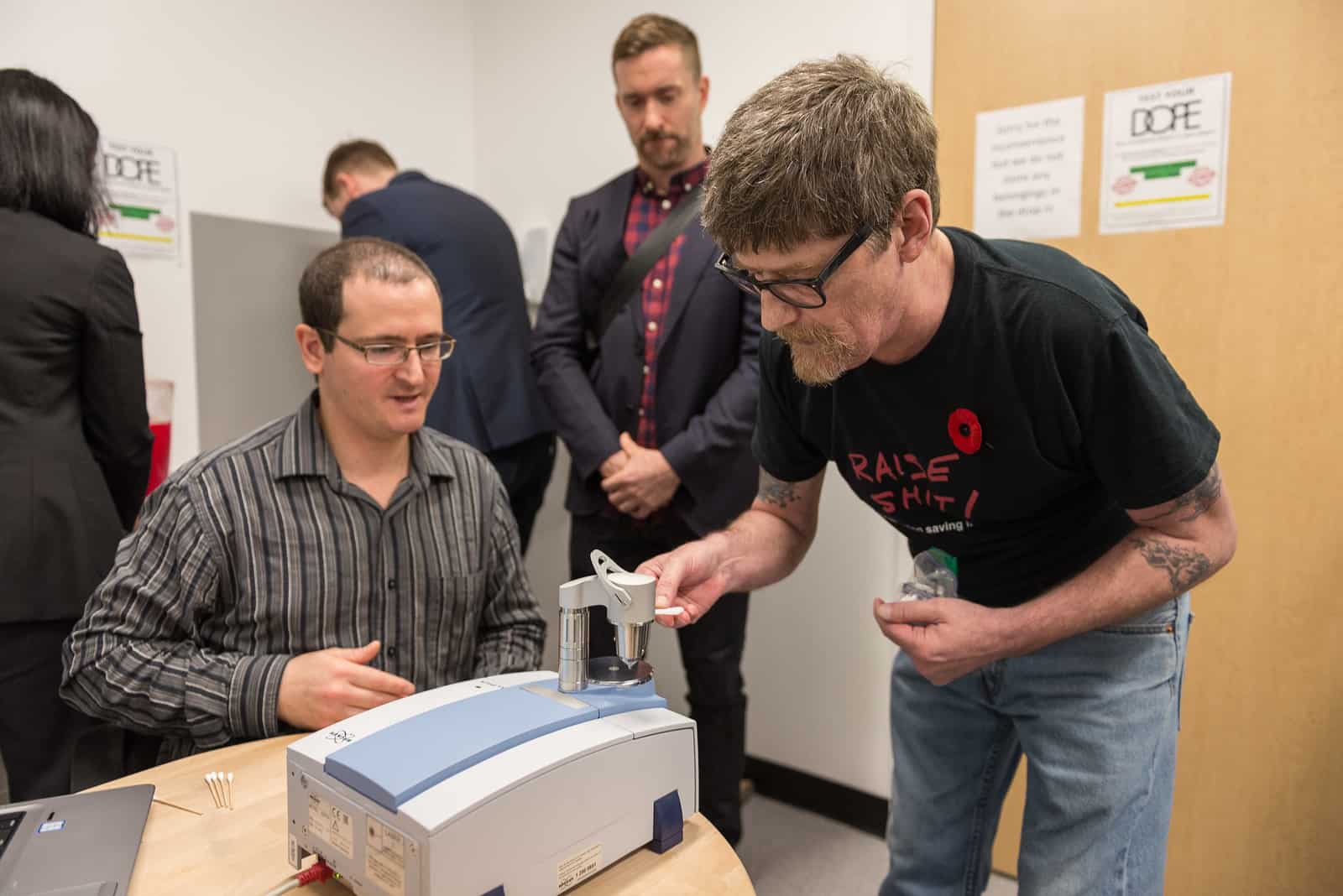
With the support of our donors, we are pioneering a new model of care for British Columbians living with substance use disorders. A model that blends evidence-based strategies, research, harm-reduction, education, and compassion.
Road to Recovery
The Diamond Foundation’s $20 million gift and the Ronald S. Roadburg Foundation’s $9 million gift to St. Paul’s Foundation will fund development of the brand-new Road to Recovery at St. Paul’s Hospital, a first-in-Canada model of care that will cut weeks on waitlists and support patients to move through a full spectrum of treatment services all in one location.
Substance use is never just about the drugs. Donors are unsung heroes of this critical work.
“Recovery isn’t just about stopping the drugs. It’s about changing your life and giving yourself permission to dream again.”
Gary L, husband, step-dad, community activist, former patient