This article is part of our continuing “Research & Innovation” series that highlights the new research and ongoing innovation that’s happening at St. Paul’s and other Providence Health Care sites.
Doctors and researchers have been on high alert from the beginning of the COVID pandemic, in part because of lessons learned 100 years ago.
- The virus that caused the Spanish flu pandemic was the most contagious and deadliest pathogen the world had ever seen: more than 500 million infected; at least 50 million dead.
- The virus came in three major waves: chillingly, the second was the deadliest.
- The majority of those who died were not elderly: they were largely between the ages of 20-50.
At St. Paul’s, doctors and researchers mobilized – even before the pandemic was officially declared – to coordinate resources, share findings, and improve the odds that patients would survive the initial infection and lessen the impact of any long-term side effects.
In May, after just one month of planning and logistics (a timeline almost unheard of in medicine), we launched our post-COVID respiratory clinic and research program. It was a great start. But we were already learning that COVID doesn’t just affect the lungs. It can have severe and lasting consequences for a patient’s heart, kidneys, brain, nervous system, and psychiatric health. Adding to the complexity of the virus, these complications can come on months after the patient has “recovered.”
It was clear we needed to cast a wide, cross-discipline net to understand the unprecedented variety of complications and to fuse immediate patient care with on-going research.
Today, a scant four months later, our post-COVID recovery clinic encompasses a team of specialists working together to address the full scope of post-COVID illness.
During a recent webinar, one of the new clinic’s principal physicians, Dr. Alyson Wong, a respirologist, and Dr. Adeera Levin, a nephrologist and senior advisor to the clinic, talked about the team’s initiatives to help patients, gather data, and find better ways to treat and prevent the complex, intertwined after-effects of COVID-19.
Patients as partners
It started by tearing down silos to consolidate the efforts of clinicians, researchers, health authorities, and universities. Now, patients who have been admitted to hospital with COVID-19 anywhere within Vancouver Coastal Health are referred to our clinics at St. Paul’s or Vancouver General.
The goal is to create a province-wide network of clinics offering patients easy access to multiple specialists and providing researchers with access to that data. Ultimately, this will help determine best practices for treating and following-up with this diverse patient group.
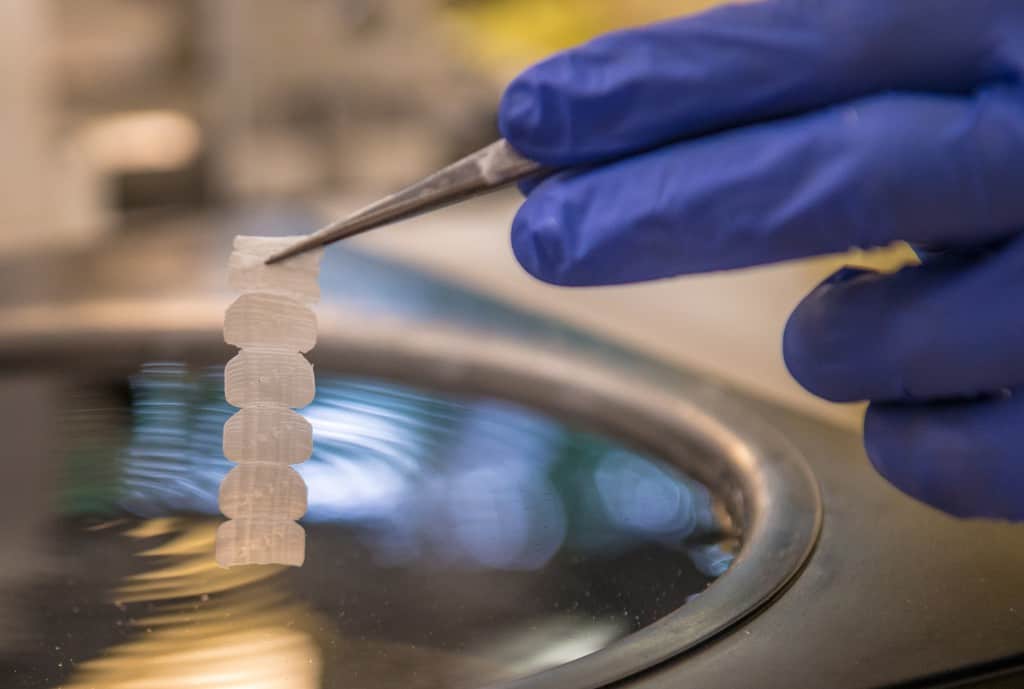
Dr. Wong is excited about the convergence of clinical care with leading-edge research. “The clinic takes patients through a standardized series of tests and comprehensive questionnaires. With their permission, patient blood and tissue samples are submitted to our biobank for further research.” Patients will return at 6, 12, and 24 months to repeat the tests and gauge their progress.
“We’ve seen 111 patients and we’re already publishing our findings,” says Dr. Wong. One of the team’s first studies was published in the European Respiratory Journal. It looked at patient-reported outcomes including on-going symptoms, frailty, psychological effects, and impact on quality of life.
Adds Dr. Wong, “These manuscripts enable us to improve care by sharing our experiences with other clinicians and researchers around the world.”
Long COVID
COVID is no ordinary virus. Researchers have started using the term “long COVID” to describe the lingering symptoms that can last indefinitely following infection.
We know that about 50% of patients who were hospitalized with COVID show a loss of lung function 2-3 months after becoming ill. “And if we look at CT chest images, nearly 90% of patients have abnormal findings,” says Dr. Wong.
In another alarming trend, evidence of chronic lung disease has been seen in COVID patients who were not critically ill and in patients who weren’t even admitted to hospital with breathing problems – they may have had gastro-intestinal issues, for example.
In addition to its impact on the body’s organs, long COVID can cause an intricate web of symptoms including chronic fatigue, ongoing muscle pain, headaches, and diarrhea. The more we learn more about these complications, the more we expand the scope of the work we’re doing at the clinic and in the lab.
Providing care beyond the hospital walls
What if chronic lung disease, debilitating fatigue, or ongoing pain are predictable consequences of surviving COVID-19? What would that mean for health care going forward? For starters, we would almost certainly see a significant increase in the number of people needing continuing care. In turn, this could become a serious burden on the health care system, not to mention patient quality-of-life.
Dr. Levin is optimistic that we can learn and adapt as we go. “We’re already rolling out solutions including a post-COVID RACE line (Rapid Access to Consultative Expertise). This made-at-St-Paul’s innovation – supported by specialists from St. Paul’s, Vancouver General, and the Fraser Health Authority – gives physicians and nurse practitioners in even the most remote corners of our province finger-tip access to specialists who can help triage and manage post-COVID complications.”
Perhaps most importantly, we’re working with, and learning from, our patients: those who have had COVID and those who are at risk to contract it. This way, we can be confident we have the knowledge and the resources to care for them now and into the future. And because this is St. Paul’s, we also have our boots on the ground helping to organize community resources and supports for patients across BC.
In the midst of an ongoing crisis, this spirit of collaboration, community, and compassion are weaving a truly hopeful silver lining.
Thanks to generous donors like you, the COVID-19 Response Fund at St. Paul’s Foundation has already donated $50,000 to support the care and research happening right now at our post-COVID recovery clinic. Be part of the silver lining, give now.