Originally appeared in the Vancouver Sun
Written by G. Marion Johnson, Postmedia Content Works
Sponsored by St. Paul’s Foundation
Anyone who’s physically active and who has been sidelined by an injury knows how frustrating that experience can be. For Maureen, a Yukon resident and carpenter, a fractured ankle bone in 1989 meant she couldn’t walk for three months or work for nearly a year. That was just the beginning of her ordeal.
Her doctor warned that the injury would make her susceptible to arthritis later in life. Sure enough, Maureen began to experience worsening pain as the years went by.
“I found it increasingly harder to function,” Maureen says. “At one point I recall it became so difficult that I couldn’t walk down the street without support. It was debilitating.”
About a decade ago, she became a patient of Dr. Murray Penner, head of the department of orthopaedics at St. Paul’s Hospital & Providence Health Care, who was consulting with a Whitehorse medical clinic as part of the team’s regional outreach. She tried assistive devices and braces to help improve ankle movement and ease her discomfort, but by 2017, her pain was unbearable.
Penner had previously mentioned the possibility of a total ankle replacement, an idea that Maureen admits terrified her. Last year, however, she proceeded with the groundbreaking surgery using new digital technology developed in part by St. Paul’s surgeons. It proved to be life-changing.
“Today, 30 years after my initial injury, I am finally active again,” she says. “I am no longer in pain. I am back doing the work I love and enjoying the outdoor activities that I have missed so much. The care, compassion, and support that I received from all the medical staff at St. Paul’s were exceptional.”
In the past, patients like Maureen with ankle arthritis were limited to options such as ankle fusion, which doesn’t always restore full range of motion, or even amputation.
When ankle replacement first came to Canada nearly two decades ago, St. Paul’s was an early adopter. The organization has gone on to be a leader, nationally and internationally, in foot and ankle surgery, which is one of the fastest-growing orthopedic subspecialties in Canada.
Research is another cornerstone of the team’s excellence, with physicians of St. Paul’s BC Foot and Ankle Clinic involved in several studies aimed at better understanding various surgical techniques to treat foot and ankle issues. Among other areas, the group has focused on patient reported outcomes of ankle arthritis in its scientific investigations.
“The impact on patients’ lives is every bit as severe if not more severe than end-stage hip arthritis, yet ankle arthritis is less well understood,” Penner says. “We’ve published the largest series of comparison studies, comparing outcomes of fusion to replacement, in the world. It’s definitely been a very active research effort locally and together with colleagues across Canada.”
In fact, expertise out of St. Paul’s has led to the design and development of the most advanced and employed total ankle replacement system in the world.
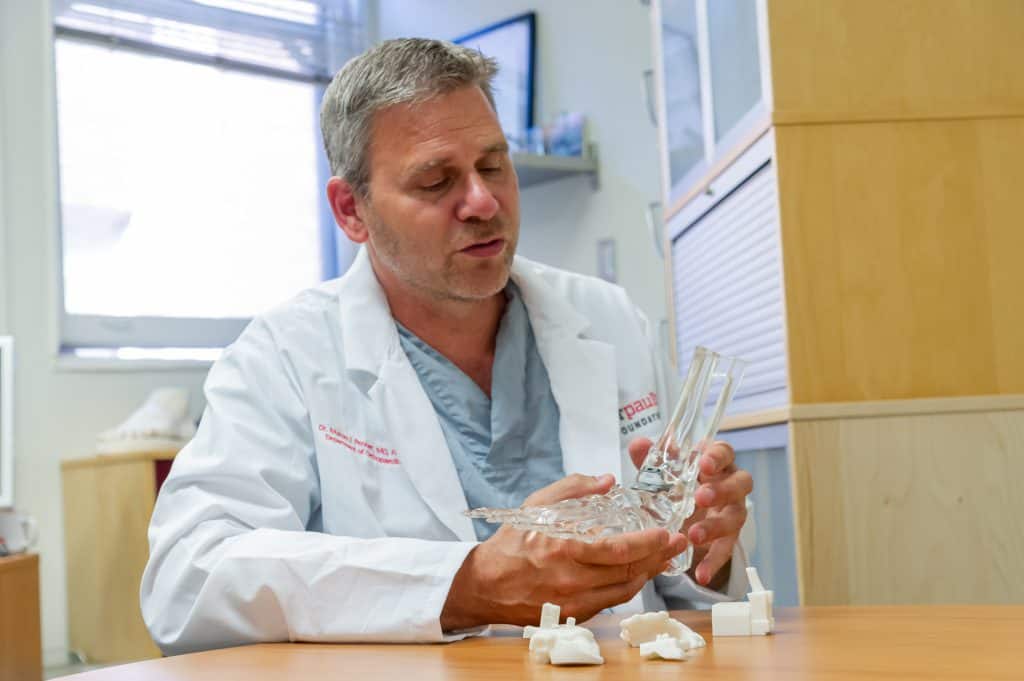
St. Paul’s surgeons co-developed leading-edge digital technology that has transformed total ankle replacement.
Here’s how it works: Images from a 3D CT scan allow for the production of a customized model of a patient’s ankle using 3D-printing technology. Doctors perform a virtual, or simulated, surgery on that model, positioning ankle implants exactly where they need to go. From there, a 3D guide sits right on the patient’s bone during the actual surgery, ensuring precise execution.
“The main key with the longevity of implant is putting it in properly, which may sound simplistic, but it’s not as easy as it sounds,” Penner says. “The 3D-printed, customized guide is patient-specific and allows us to do surgery far more accurately and quickly. Many of our cases are complicated, and if we can save time on that aspect—the placement of the implants—it gives us more freedom and time to deal with complex aspects of surgery.
“The 3D guidance system has changed the way ankle replacements can be done,” he adds. “The end result for Maureen has been fantastic.”
The other crucial component of successful total-ankle replacement is what’s called a Mini C-Arm Scanner. Although these devices have been in use for several years, technology has advanced, making them smaller and easier to use, benefiting patients and physicians alike.
“New scanners have been introduced recently with vastly improved resolution and larger imaging capture fields, significantly improving accuracy and the ability to visualize the procedure,” Penner says. “In addition, they have significantly less radiation output than large C- Arms, reducing radiation exposure to the patient and medical staff in the room.”
Doctors can also use the Mini C-Arm Scanners to perform minimally invasive surgery through a small incision area guided by digital imaging. This technique reduces surgical and recovery time.
Mini C-Arm Scanners are typically fairly expensive, however, requiring significant capital outlay. Donor dollars help make these kinds of innovations possible.
“The hospital relies heavily on donor finding to support capital-purchase initiatives such as a Mini C-Arm,” Penner says. “If it were not for the support of our donors, this technology would not be available to our patients.”
To support the work of St. Paul’s orthopedic team and help patients like Maureen through the purchase of a Mini C-Arm Scanner, please give now.
This story was created by Content Works, Postmedia’s commercial content division, on behalf of St. Paul’s Foundation.