Blankets are cherished essentials for newborns, providing warmth, comfort, and security. At St. Paul’s Hospital, a special kind of blanket – the bili blanket – is helping babies recover from jaundice quicker and allowing more time for skin-to-skin contact and cuddles with their parents.
The Pregnancy, Birthing, and Newborn Centre at St. Paul’s Hospital welcomes 1,200 babies to the world every year. About 14% of those babies are born with jaundice, a common condition in newborns that occurs when bilirubin builds up faster than a baby’s liver can break it down.
While a serious and potentially fatal condition in the past, today jaundice in newborns is easily treatable. The traditional treatment is phototherapy (light therapy), where light waves absorbed by the baby’s skin and blood break down the excessive bilirubin so it can be eliminated in the baby’s stool.
The downside of light therapy, however, is that the baby must be placed in an incubator. This means separating the parent and baby only a couple of days after birth. In 2016, thanks to generous donors, St. Paul’s Hospital purchased its very first bili blanket. And it’s been a revelation for newborns, parents, and staff.
What is a bili blanket and how does it help?
The bili blanket is a portable, fibre-optic blanket providing UV phototherapy for infants with severe jaundice, used in conjunction with standard incubator phototherapy. Babies lie down on the blanket, with its lights wrapping around their backs while they receive additional light therapy from the incubator lights above them. This extra light coverage often helps babies recover faster.
One of the most critical benefits of the bili blanket is it can continue necessary treatment when the baby is out of the incubator, promoting bonding between newborns and parents or caregivers.
The baby can be held, fed, and rocked throughout the bili blanket therapy session, without interrupting the benefits of skin-to-skin contact. It promotes a nurturing environment that encourages and supports healthy and healing interactions.
Nurse Clara Vuong, who’s worked in the neonatal intensive care unit (NICU) for 18 years, has noticed a significant difference in young patients since the bili blanket’s introduction to the department in 2016. Bilirubin levels drop much quicker now.
“The bili blanket is one of our most-used pieces of equipment,” she says. “There is a huge benefit to using them for these babies.”
Full Circle: A nurse’s path from care provider to grateful parent
For the last four years, Pregnancy, Birthing and Newborn Centre nurse Julia Wulffhart has used bili blankets with young patients and their parents almost every week. She loves that they’re simple to use, incredibly effective, soft on a baby’s delicate skin, and helps reduce parental stress.
“The whole setup can sometimes look daunting. There’s the incubator and these big bulky lights, and the blue light can take over the room,” she says. “The blanket is really easy for parents, and much less overwhelming.”
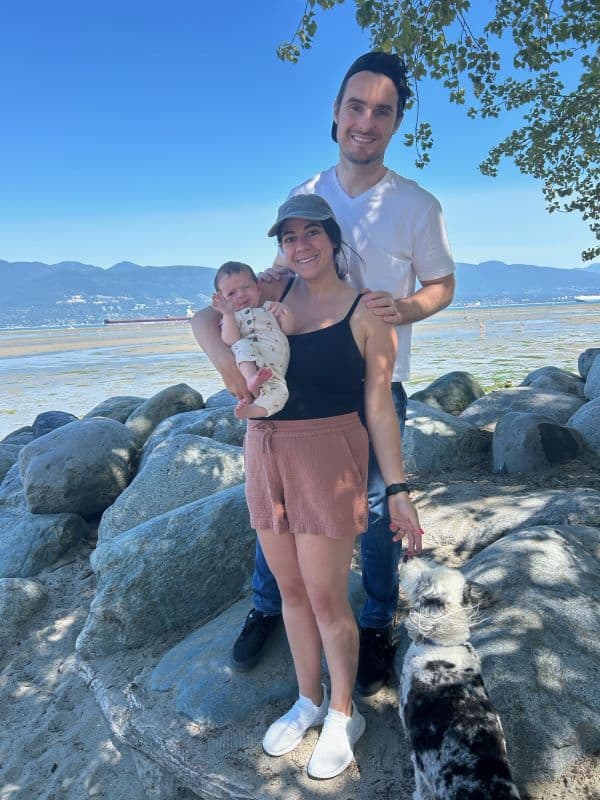
Bili blankets also played a vital role in alleviating Julia’s anxiety as a new parent. When her daughter was born with a case of jaundice that took longer to heal, they were hospitalized for an entire week and Julia was able to use the blanket throughout their stay.
“I was really grateful we had the blanket,” she says. “Being able to bring her out and use the blanket while I was breastfeeding allowed me to have a little bit more bonding time with her. I really needed that for my emotional state, knowing what I know about benefits of skin-to-skin and bonding.”
Enhancing the baby-friendly initiative at St. Paul’s Hospital

The benefits of the early skin-to-skin bonding period are numerous as babies transition to life outside the womb. They stay warmer. They cry less. They have lower levels of stress hormones. They are likely to breastfeed sooner. They are even exposed to germs on their parent’s skin that help build up their natural defense systems.
In 2023, St. Paul’s Hospital was the first hospital in British Columbia to achieve accreditation as a baby-friendly hospital, a recognition of its efforts to instill best practices in infant feeding. It’s one of only 20 Canadian hospitals to achieve this designation.
“Skin to skin is super important in the beginning and using the bili blanket really helped me to connect with my daughter while she was being treated,” says Julia. “The unit’s really proud to be a BFI-accredited hospital and the bili blanket lights really help maintain that.”
Thanks to donors and participants in the Lights of Hope Raffle, the collection of bili blankets at St. Paul’s Hospital has now grown to six, which are shared between the maternity and NICU units.
“The generosity of donations that have enabled us to purchase these blankets has been huge,” Clara says. “It gives us the ability to readily access better phototherapy treatment, and I can’t emphasize enough how helpful it has been for our babies.”
When you give to Lights of Hope, you help families during some of life’s toughest moments. And you help support innovative research that saves and improves lives.
