Meet Kathryn.
Kathryn and her husband Greg live in Daajing Giids (formerly the Village of Queen Charlotte) on Haida Gwaii. Kathryn is an active 70-something, a yoga teacher, and a former community health nurse. When she suddenly developed chest pain and began feeling weak and short of breath, she knew something was wrong, but she hoped it would go away. It didn’t.
“I’m very fit and healthy. I didn’t believe I could be having heart issues.”
Meet Dr. Tracy Morton.
You could say Dr. Morton is a unicorn: he’s a family doctor. For 22 years, he’s been part of a small, multi-disciplinary team caring for the 2,500 people who live in Daajing Giids and the communities at the south end of Haida Gwaii.
“Practicing here is really diverse and rewarding. But, we’re not equipped for advanced diagnostics. We can do lab tests. We can take X-rays. But that’s about it.”

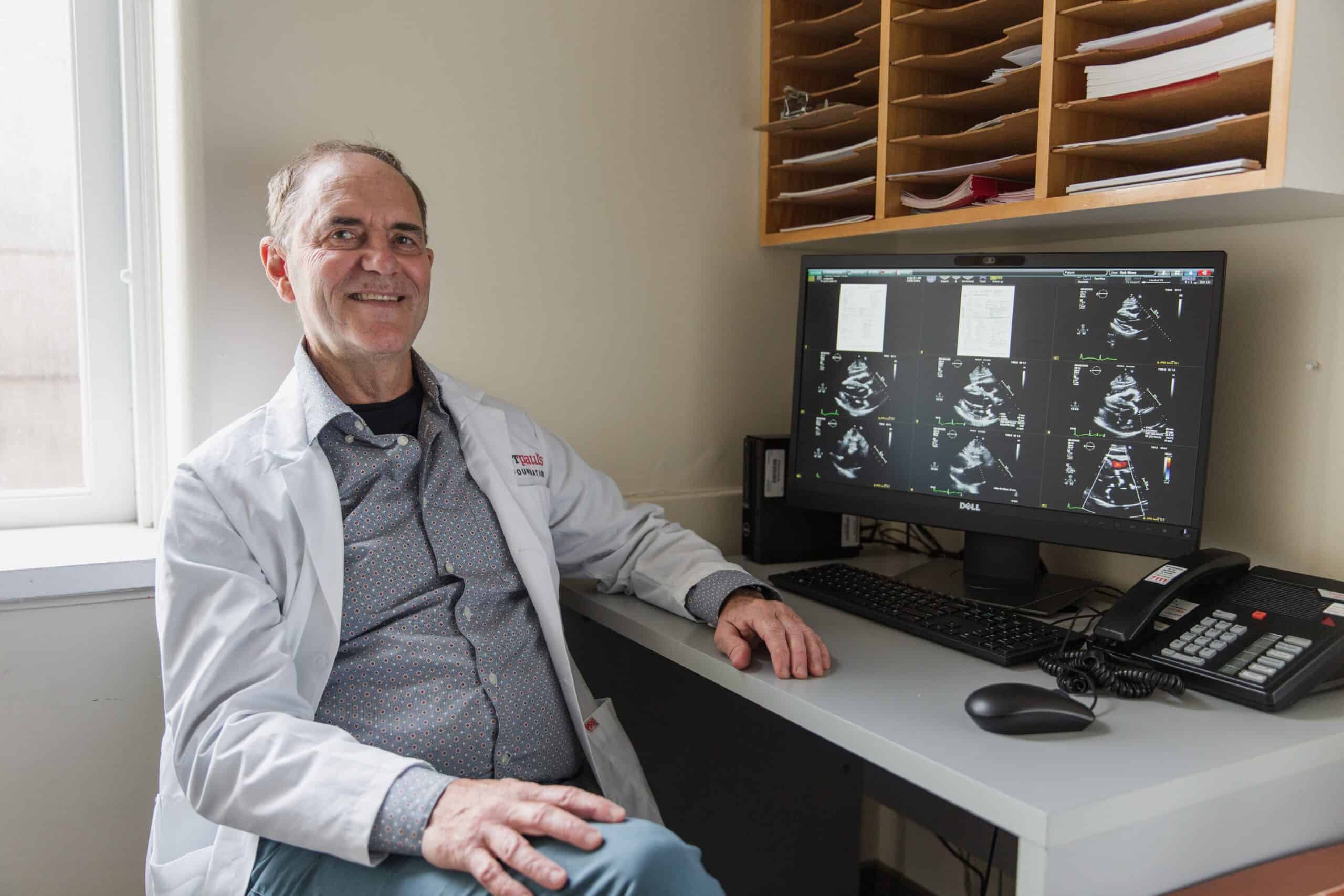
Meet Dr. Rob Moss
Dr. Moss is a cardiologist. Originally from Australia, he came to St. Paul’s in 2005 to do a fellowship in echocardiography (ultrasound of the heart). He’s been here ever since. As a doctor who specializes in ultrasound and cardiac care, Dr. Moss was in the right place (St. Paul’s) at the right time (this past spring).
“Tracy called me out of the blue one day and told me he needed my help.”
What if the help you need is hundreds of kilometres away?
Kathryn waited a full week for her pain to go away. Instead, it got worse. She went to the emergency room. Her symptoms seemed to point to a blood clot in her lung. But without a specialist or a CAT scan to confirm, Dr. Morton referred Kathryn to the hospital in Terrace for further testing.
As the crow flies, Terrace is only 265 kilometers. But in real life, it’s considerably further. If the weather, the roads, and the ferry all cooperate (and that’s a big “if” for most of the year), it takes about 11 hours. Each way.
Unfortunately, Kathryn’s tests gave Dr. Morton more questions than answers. That’s when he reached out to Dr. Moss.
Together, they came up with a plan that included the breakthrough imaging technology, an iPhone, and FaceTime.
This won’t hurt a bit
The breakthrough imaging technology is called PoCUS and it stands for Point of Care Ultrasound. It’s a small, wireless “scanner” that takes ultrasound pictures and video inside almost any part of the body and displays them on any mobile phone or tablet.
Picture this:
- Dr. Moss at St. Paul’s in Vancouver;
- Dr. Morton, in Haida Gwaii listening to Dr. Moss’ instructions and maneuvering the PoCUS wireless scanner across Kathryn’s chest;
- Greg, holding his iPhone and streaming real-time images of Kathryn’s beating heart back to Dr. Moss.
It sounds like science fiction! Dr. Moss could see exactly what was wrong: Kathryn had a failing heart valve and a life-threatening build-up of fluid and inflammation around the lining around her heart.
That’s why her tests were inconclusive. “She had two very different diagnoses. They didn’t fit into a neat bundle,” says Dr. Moss. “She needed urgent treatment beyond the scope of what was available in Haida Gwaii or Terrace.”
Kathryn was rushed to St. Paul’s the next day. Even though she was in critical condition, she remembers feeling like she was in a safe cocoon.
“I’ve almost never been a patient,” she says. “I can’t believe how comforting it was to have all of these people around me, caring for me. And was the middle of COVID, but everyone was still so patient and kind.”
Today, Kathryn and Greg are back home. She’s almost back to her old self with an active routine that includes a daily 5K hike. “She’s almost catching up to me,” laughs Greg!
Dr. Morton has become an even bigger fan of PoCUS and of St. Paul’s. “If you’re a patient in rural BC, St. Paul’s is your acute care hospital. Kathryn was in severe heart failure. Without PoCUS, Dr. Moss, and St. Paul’s, she wouldn’t have received the treatment she needed. She would have died.”
Dr. Moss has equally high praise. “It’s very challenging to get useful images during a heart ultrasound. But together, we did it.” Now it’s his turn to laugh. “As we were examining Kathryn – almost 1,000 kilometers apart – Tracy said ‘I think I’m seeing the future!’ He’s right. This is a fantastically exciting time.”
It’s amazing how much a non-invasive procedure like ultrasound can reveal!
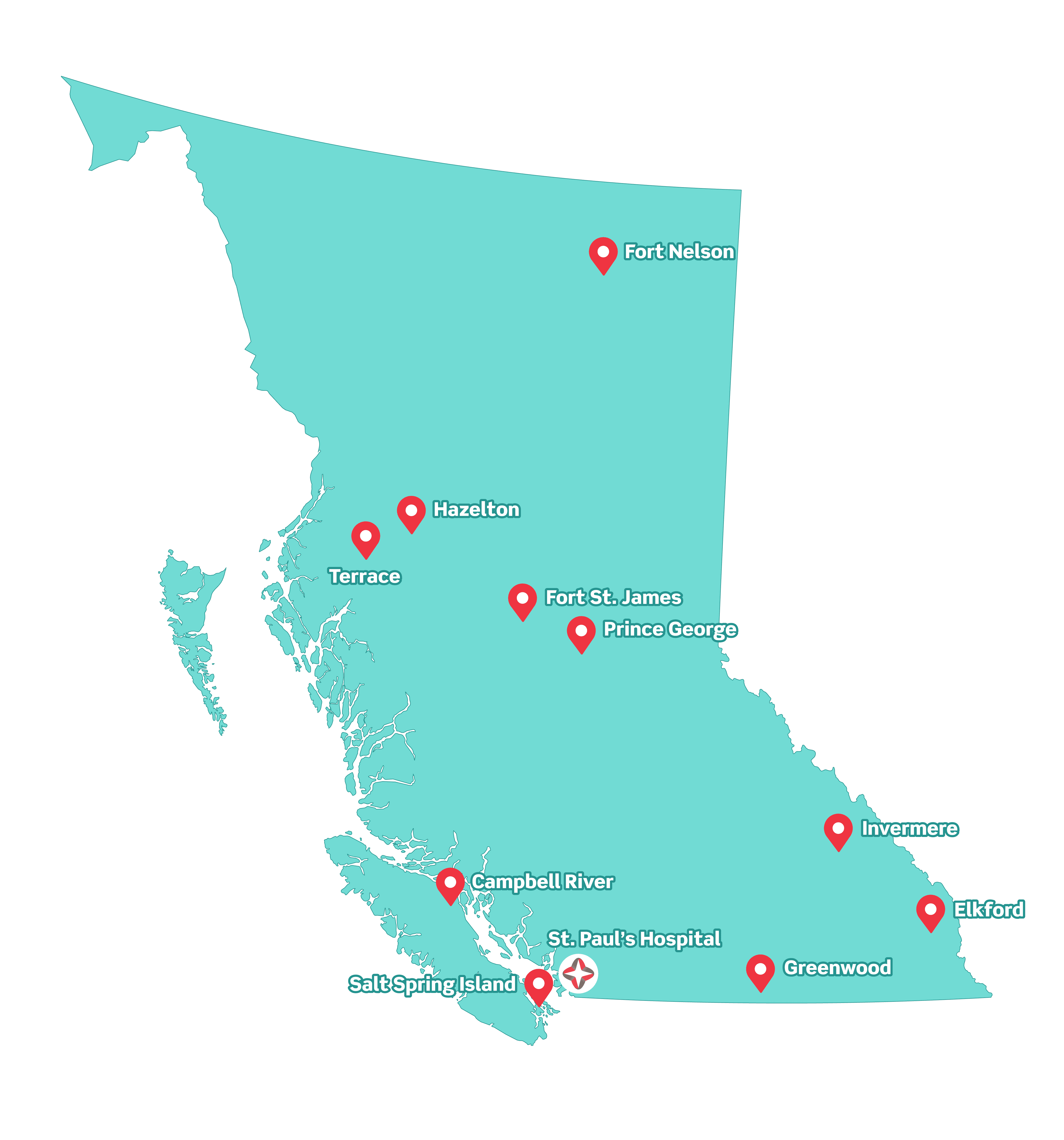
More than 600,000 British Columbians live in rural communities and small towns. They need the same quality care as their big city counterparts. PoCUS can mean the difference between life and death.
It did for Kathryn. From the onset of her symptoms to her life-saving surgery, was just 5 weeks. Her story has a happy ending thanks to the technological breakthrough of PoCUS, the collaboration of world-class specialists at St. Paul’s, and the support of generous donors like you!
Asked what she’s doing now that she wasn’t doing when her symptoms started, Kathryn’s voice catches. “Feeling grateful,” she says.
Believe it or not, PoCUS and the cloud-based network that supports it, were made possible because of your donations! It’s an initiative of Canada’s Digital Technology Supercluster, of which Providence Health Care is a founding member. With impressive speed, Providence Health Care, Change Healthcare, Clarius Mobile Health, the University of British Columbia, St. Paul’s Foundation, and the Rural Coordination Centre of BC joined forces to deploy portable handheld ultrasound scanners in remote communities across the province.
Your gift to Lights of Hope brings PoCUS and innovative patient care to all British Columbians. Your support saves lives like Kathryn’s! On behalf of the people who live in BC’s remote and rural communities, thank you!
