This article is part of our continuing “Research & Innovation” series looking at some of our most exciting studies, breakthroughs, and discoveries.
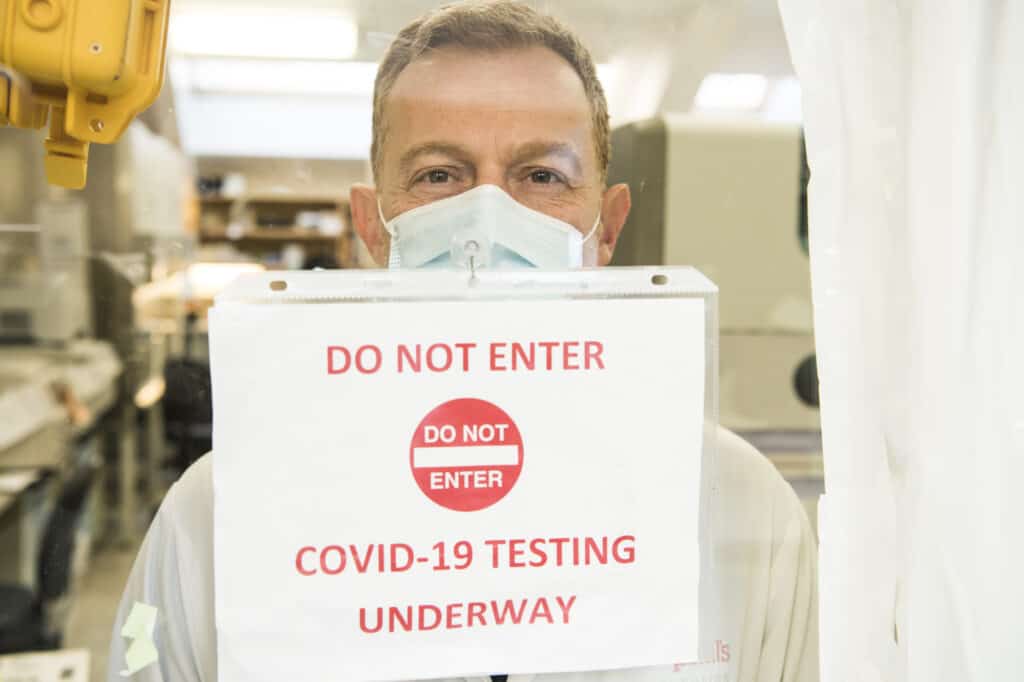
Our lab puts the labor in laboratory
“For two full years, our laboratory’s technologists and doctors have literally worked day and night to deliver accurate, timely results,” says Dr. Marc Romney. This commitment has been critical to public health and clinical decision-making across BC and Yukon.
Here are a few highlights.
- Since February 2020, our lab has performed almost half a million (!) PCR tests.
- We have one of Canada’s most comprehensive COVID testing menus including: PCR testing (using 6 different technologies), sequencing of the SARS-CoV-2 virus, and SNP testing (to quickly identify variants of concern).
- We are leading a research team investigating COVID-19 immunity and infection among older adults, including antibody responses after vaccination in long-term care residents.
- We are working with the WHO and others to advance international standardization of antigen testing (rapid testing).
Post-COVID Respiratory Clinic shares one-year findings
The team at our Post-COVID Respiratory Clinic is set to publish a paper highlighting the results of their first year-long patient study into how respiratory tests and patient symptoms change over time during COVID recovery. If this is the first you’re hearing about the clinic, it’s part of a broad, post-COVID network staffed by a multidisciplinary team of specialists working together to treat and research the full scope of post-COVID illness. (Read more about their innovative approach here.)
We asked Dr. Alyson Wong, one of the clinic’s respirologists, for more details.
“We’ve seen close to 150 patients now,” says Wong. “And we’re struck by the number of patients with persistent symptoms.”
The team has collated a significant body of research in an attempt to find out why some people have such prolonged symptoms.
For example, in patients who were hospitalized with COVID, lung function improved between 3 and 6 months. But by 12 months, the improvements had stopped. And despite nearly-normal breathing and imaging tests, 60% of patients reported ongoing symptoms (persistent shortness of breath, cough, frailty, and poor sleep and mood) a full year later.
“The causes of these persistent symptoms are still poorly understood,” says Wong.
She explains that, so far, treatments have mainly consisted of testing and treating for other causes that could be contributing to symptoms, education (for example, explaining test results and discussing strategies on returning to work or exercise), and anti-inflammatory medications.
Although there aren’t a lot of treatment options (yet), Wong says the patients have embraced the opportunity to be part of this groundbreaking research. “They really appreciate being tested for their specific symptoms and having the chance to discuss their concerns and their progress with our specialists.”
A breakthrough for women with fibroids
Fibroids are common benign tumors that grow in the muscular wall of the uterus. If you have them, your period becomes heavier and more painful and you can experience anemia and chronic pelvic pain. In some cases, fibroids can even lead to infertility or problematic pregnancies. And they’re responsible for about one-third of the 60,000 hysterectomies performed in Canada each year.
But now, thanks to Dr. Fariba Mohtashami, there’s a new, safer, less invasive alternative. Using a minimally-invasive laparoscopic technique (sometimes called keyhole surgery), the surgeon can remove large fibroids through small incisions, without removing the entire uterus.
“Diseases affecting female reproductive organs are among the least studied in the human body,” Mohtashami says. “And fibroids are no exception.” However, with proper training and access to up-to-date operating rooms, equipment, and hospital resources, up to 96% of hysterectomies – and the majority of fibroid removals – can be done through laparoscopy, rather than big cuts.
“Patients lose less blood during surgery, form less scar tissue, and return to their normal lives far sooner with this technique than those who’ve undergone open surgery,” she adds. “In fact, it’s not uncommon for patients to go home the same day.”
Mohtashami submitted a video of the technique (as an educational resource guide for other surgeons) to Canadian Society for Advancement of Gynecologic Excellence (CanSAGE). CanSAGE was so impressed, it was named Canada’s top video in the category of “Practical Education Technique.”
Putting our best foot (and ankle) forward
Ankle arthritis is one of the leading causes of chronic disability in North America. The good news is, Providence is a world leader in foot and ankle surgery. Dr. Alastair Younger is leading the team to pioneer some exciting advances in ankle arthritis and joint replacement surgery.
“We have the only weight-bearing CT scanner in Canada,” says Younger. “That allows us to get extraordinarily detailed, high-res images of the foot and ankle bones.” Before surgery, the scanner is used to assess and map exactly what needs to be done. Afterwards, it allows the team to see how the bone is healing and to prevent the patient from needing further surgical intervention.
In another significant first, Younger has developed a minimally-invasive technique for arch reconstruction using “stab incisions” (exactly what it sounds like: multiple, tiny openings in the skin).
“One of the biggest risks with this surgery is infection,” Younger says. “So the smaller the incision, the less chance there is for complications.” Providence is the first and only place in the world using this approach.
Research is another area of distinction for Younger and the team. With more than 800 patients enrolled in various studies, they’re studying things like gender differences in surgical outcomes and the long-term benefits of ankle replacements vs. fusion and open vs. arthroscopic surgery.
“So while we’re replacing ankles, we’re also trying to understand the true science behind the regeneration of bone and skin and how we can arrest arthritis progression.”
“The goal is to help people heal in a shorter period of time. After all, the more you heal, the less you hurt.”
By Kris Wallace
Special thanks to our physicians!
Dr. Marc Romney, head, Medical Microbiology and Virology, St. Paul’s Hospital/Providence Health Care; clinical professor, UBC
Dr. Alyson Wong, respirologist, St. Paul’s Hospital; clinical assistant professor, UBC
Dr. Fariba Mohtashami, head, Division of General Obstetrics & Gynecology, St. Paul’s Hospital; clinical associate professor, UBC
Dr. Alastair Younger, orthopedic surgeon and senior director of foot and ankle research at Providence Health Care
Thanks to generous donors like you, innovation and research go hand in hand. Your gift today helps our clinician-researchers continue their life-changing work. Give today.